New Cholesterol Guidelines From A Neurologist’s Perspective
The American Heart Association’s annual premier conference “Scientific Sessions 2018” concluded on Monday. This meeting showcases the latest advancements and discoveries in the field of cardiovascular medicine and is attended by clinicians and researchers from across the world.
Being a vascular neurologist, I have attended the International Stroke Conference organized by the AHA several times, however, this was my first time attending Scientific Sessions. I was able to attend the conference via Live Streaming while sitting in my office in Burlington, Massachusetts.
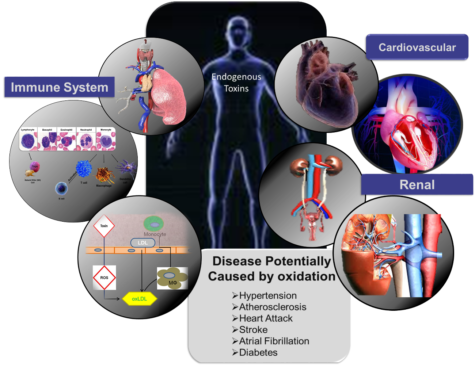
There are a lot of overlaps between cerebrovascular and cardiovascular disease and I was particularly interested in attending the sessions pertaining to stroke prevention and brain health. One of the most anticipated presentations was the release and discussion of the new AHA/ACC Cholesterol Clinical Practice Guidelines.
Some key takeaways from the updated guidelines:
- The guidelines continue to underscore the role of lifestyle and dietary habits in addition to lipid lowering medication use to treat cholesterol disorders. There is emphasis on the concept of shared decision making with the patient which should include discussion of their individual risk and the treatment options to reduce that risk.
- Addition of Ezitimibe and subsequently PCSK-9 inhibitors is now recommended in patients who cannot achieve target LDL levels despite maximum tolerated statin doses. There is some concern about the cost effectiveness of PCSK-9 inhibitors, but these medications are expected to become cheaper in the future.
- Risk enhancing factors are introduced as part of a personalized approach to risk assessment prior to initiating statin therapy. These include persistent elevation of LDL>160 mg/dL, history of pre-eclampsia, family history of premature atherosclerotic cardiovascular disease, history of chronic kidney disease and chronic inflammatory disease, among others.
- There is a recommendation for expanding use of calcium score as part of the risk assessment, especially in patients where risk benefit analysis is uncertain.
In addition to the guidelines for medications and lifestyle changes to treat cholesterol disorders, I especially enjoyed Dr. Laurence Sperling’s talk about the safety of statins.
Patients should be prescribed statins again at a lower dose or modified drug regimen if the reason for discontinuation was mild side effect symptoms. Although rare, but some patients do develop severe myopathy with statin use. These patients should be prescribed alternate non-statin therapies to achieve the target cholesterol levels. There has not been any proven benefit of Co Q10 to prevent or treat statin associated muscle symptoms. Despite the increased risk of diabetes mellitus with statins, it is recommended to continue the drug in patients who may be at risk or develop new onset DM. These patients should be counseled about the net clinical benefit of these drugs for long term cardiovascular event prevention. It appears reasonable to initiate statin therapy in the presence of an appropriate indication despite a history of stable liver disease. In patients without hepatic disorders, there is no clinical benefit of routine creatine kinase and liver enzyme measurements.
Very often patients have questions and concerns about initiating and continuing their statin medication. I believe that these data and recommendations further reinforce my personal practice to encourage patients to continue their statin medication as the risk benefit ratio remains favorable despite mild side effects.



 The months of March and April were filled with a whirlwind of conferences. I had the pleasure of traveling to several meetings across the U.S. including the
The months of March and April were filled with a whirlwind of conferences. I had the pleasure of traveling to several meetings across the U.S. including the