Highlights of AHA18 – Bridging Lifestyle Medicine with Contemporary Medicine through Science
This year’s annual scientific meeting of the American Heart Association (AHA) held in Chicago, Illinois November 10-12, 2018 was excellent. The abbreviated 3-day meeting received positive feedback as this allowed practicing physicians to attend the meeting over the weekend and be able to return to their practice early in the work week rather than having to spend an extended time away from the office. It was great being a part of the AHA Early Career Blogger group as this allowed access to many of the embargoed sessions. At these sessions I was able to listen to the AHA 2018 updated Lipid Management Guidelines1 as well as The Physical Activity Guidelines for Americans, Second Edition2 prior to their release at the meeting. This gave me a chance to ask the guideline committee several questions related to patient management.
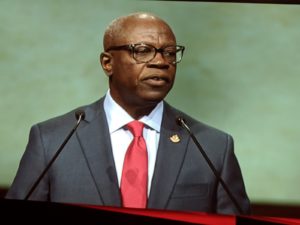
Opening Session:
The opening session by Dr. Ivor Benjamin, the President of the American Heart Association, delivered very powerful messages throughout his speech. He highlighted the track of his career and the important role of strong mentors throughout his career and the impact it had on his advancement throughout the field of cardiology. He also discussed both the importance of mentoring and diversity in the cardiology profession highlighting the fact that African American men account for only 3% of Cardiologists in the United States and the need to bridge this gap. I found this session very inspiring and encouraging especially with regards to mentoring and supporting junior colleagues and being grateful for the mentors I have had thus far in my career. I also welcomed the message of the importance of diversity and inclusion as this leads to a healthier work and training environment.





Bridging Lifestyle Medicine with Contemporary Medicine through Science:
This year’s meeting highlighted the value of integrating lifestyle medicine with contemporary medicine to achieve the best outcomes for patients with regards to the prevention of cardiovascular disease. This was supported by the release of the updated 2018 American College of Cardiology (ACC)/American Heart Association (AHA) Guidelines on Lipid Management on the first day of this meeting1. This updated guideline emphasized the importance of the cholesterol management at all stages of adulthood along with the importance of therapeutic lifestyle changes1. The utility of coronary artery calcium (CAC) scoring with cardiac CT was also emphasized as a useful tool to further refine patients’ risk to determine the best management for patients who are at intermediate risk for atherosclerotic cardiovascular disease (ASCVD)1. This guideline also had included ezetimibe and PCSK9 inhibitors as having a complementary role when used with statin therapy in selected patients at high risk for ASCVD1. The release of this updated guidelines will be a useful in my management of patients with regards to primary and secondary prevention of ASCVD. I appreciated the role of CAC scoring which will be very helpful for the management of the intermediate risk patients.
The release of the U.S. Department of Health and Human Services’ second edition of the Physical Activity Guidelines for Americans on the last day of the meeting was also well received2. This second edition emphasized the importance of increasing physical activity for all age ranges throughout the population including women in pregnancy and the postpartum period, as well as adults with chronic diseases or disabilities2. This guideline update will assist me with counseling patients with regards to increasing their physical activity to improve their overall cardiovascular health.
Networking Opportunities:
There were many networking opportunities during the meeting. These included the Council on Clinical Cardiology dinner on the first night of the meeting which honored Dr. Judith Hochman the recipient of the James B. Herrick Award for Outstanding Achievement in Clinical Cardiology. Dr. Stacy Rosen was also the recipient of the Women in Cardiology Mentoring Award. This dinner was attended by many leaders in the field of Cardiology and was a great opportunity for me to meet these leaders. The Women in Cardiology Committee also hosted a networking luncheon on the first day of the meeting during which Dr. Sharonne Hayes from the Mayo Clinic was the keynote speaker. Dr. Hayes gave a very riveting interactive talk on leadership for women in cardiology, she was also the recipient of last year’s Women in Cardiology Mentoring Award. Her talk was useful with very powerful messages on navigating your professional and personal life to achieve overall job satisfaction, career success and personal happiness. I learned several tips that I will apply to my own career as well. Dr. Annabelle Volgman and the faculty at Rush University was gracious to host a wonderful networking dinner for Women in Cardiology (WIC) on the second night of the meeting. This dinner provided a great opportunity for me to meet fellow WIC colleagues and to discuss several relevant issues related to our practice in the Cardiology field.

Social Media Coverage:
There was also a broad social media coverage of the meeting on Twitter and this was assisted by the AHA Early Bloggers writing group. I was able to share live tweets during several sessions and this generated a lot of discussion amongst members on Twitter. This also allowed many colleagues who were unable to attend the meeting to be able to follow and comment on several meeting highlights.
Looking Forward to AHA 2019:
This year’s AHA Scientific Sessions embrace of lifestyle medicine and the value of preventive cardiology was refreshing and empowering. This meeting highlighted the importance of not only treating ASCVD but also the importance of preventing disease and empowering our patients to take responsibility for their health as well. In the words of Goethe as mentioned in Dr. Ivor Benjamin’s opening session “Choose well….your choice is brief, and yet endless.” We look forward to next year’s AHA 2019 meeting in the beautiful city of Philadelphia.
References:
1. Grundy SM, Stone NJ, Bailey AL, Beam LT, Birtcher KK, et al. 2018AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. JACC Nov 2018, 25709; DOI: 10.1016/j.jacc.2018.11.003
2. The Physical Activity Guidelines for Americans: THe HHS Roadmap for an Active Healthy Nation. Second Edition. ADM Brett P. Giroir, MD.