What Are the 7 Steps to A Heart Healthy Lifestyle
The key ‘take home’ points for patients based on the latest 2019 American College of Cardiology (ACC)/American Heart Association (AHA) Guidelines on Primary Prevention of Cardiovascular disease.
Introduction
Following the theme of Preventive Lifestyle from the 2018 American Heart Association meeting, EPI | Lifestyle 19, the Cardiology community eagerly awaited the release of the highly anticipated 2019 American College of Cardiology (ACC)/American Heart Association (AHA) Guidelines on Primary Prevention of Cardiovascular disease1. These guidelines were released at the recent ACC annual scientific meeting in New Orleans, Louisiana March 16-18, 2019. There is an increased focus on the importance of lifelong adherence to a heart healthy lifestyle of eating heart healthily and maintaining a physically active lifestyle. There were also new recommendations with regards to use of aspirin for primary prevention. These recommendations have caused some anxiety with regards to use of aspirin, a common drug used by many persons over the last several decades hoping to prevent heart disease. Cardiologists have already received questions from their patients regarding aspirin use and the recently release prevention guidelines. In this blog I will focus on the key take home messages for patients from these prevention guidelines and the seven steps to heart healthy living outlined in the guidelines.
Where should I begin?
A heart healthy lifestyle is one that is important to start at any age, and the earlier this is started in life, the better the degree of prevention. Living a heart healthy lifestyle should first begin with an assessment of your cardiovascular (CV) risk which is defined as the probability/chance of an individual having a cardiovascular event, such as a heart attack or stroke, over the next 10 years. CV risk is based on family history of premature heart disease, age, gender, ethnicity, history of tobacco smoking, level of physical activity, diet, the presence of diabetes, hypertension and/or hyperlipidemia.
Your CV risk should be assessed by your physician. Based on your history, physical exam and blood testing, a CV risk profile can be assessed and calculated based on the ACC AHA CV risk calculator. After your risk is calculated, your physician can customize their recommendations based on your CV risk profile. Most times further testing may not be necessary. However, for individuals with an elevated CV risk score further testing may be recommended. These tests may include a Cardiac CT scan without contrast to assess for the presence and degree of calcification of the blood vessels of the heart, which suggests the presence of hardening of the blood vessels known as atherosclerosis. This atherosclerosis indicates a high CV risk as it is a usual precursor for heart attacks and strokes and for patients with this finding further treatment and/or testing may be recommended by your physician.
Next steps
There are 7 main take home messages for healthy individuals preventing heart disease, the first three steps are focused on living a healthy lifestyle. The last 4 steps focuses on recommendations related to medical therapy and should be actively discussed with your provider to customize recommendations based on your CV risk profile.
Step 1 – Heart Healthy Diet
A diet that is focused on eating fresh fruits, vegetables, legumes, nuts and whole grains is recommended. Sweetened drinks, processed foods, foods with a high content of sodium, and foods containing trans fats and saturated fats should be avoided.
Step 2 – Physically Active Lifestyle
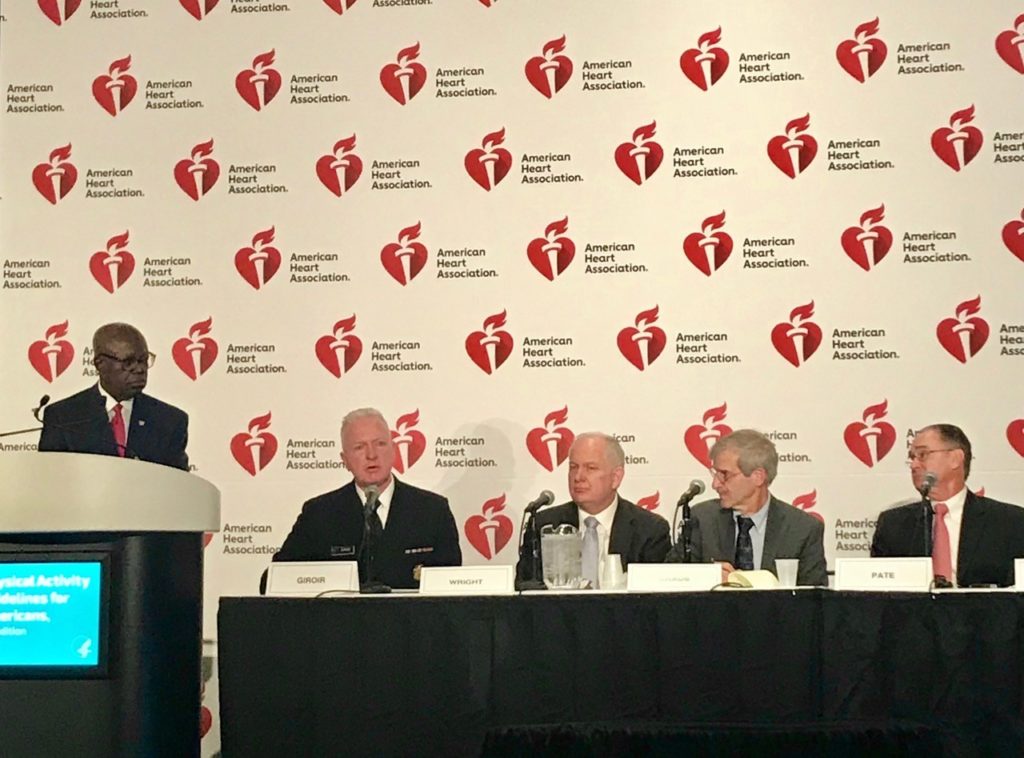
Maintaining a physically active lifestyle is also recommended with at least 150 minutes a week of moderate intensity exercise such as a brisk walk or 75 minutes a week of high intensity exercise such as playing basketball, rowing, et cetera. Generally, maintaining physical activity should be a daily regimen rather than focused on 1 or 2 days a week which was emphasized in the 2018 updated second edition of the Physical Activity guidelines that were released by the Department of Health and Human services2.
Step 3 – Cessation of Tobacco Smoking
Tobacco smoking is the single most potent reversible risk factor for cardiovascular disease. It is recommended that tobacco smoking is avoided to prevent the development of cardiovascular disease. This recommendation is relevant for all age groups.
Step 4 – Maintaining Healthy Cholesterol Levels
Your cholesterol levels should be checked by your physician on a regular basis as determined by your provider and latest guidelines. Based on your individual CV risk, your physician may opt to start medical therapy to manage your cholesterol or may opt to perform further testing such as a non-contrast Cardiac CT to determine calcifications in the blood vessels of the heart reported as a “CAC score.” This CAC score will assist your physician to determine the need for medical therapy and/or further testing.
Step 5 – Maintaining a Healthy Blood Pressure
Achieving and maintaining a healthy blood pressure of <130/80 is recommended. This may or may not require medical therapy as determined by your physician. A physically active lifestyle, low sodium diet and a diet rich in fruits and vegetables are helpful in maintaining a healthy blood pressure.
Step 6 – Maintaining a Healthy Glucose level and Adequate Control of Type 2 Diabetes Mellitus (DM)
Adequate control of type 2 DM is important to prevent cardiovascular disease. A heart healthy diet as outlined previously in this blog along with one that is low in sugar and processed foods, as well as maintaining a physically active lifestyle, are vital in controlling DM. Additionally for diabetic patients on medications, Metformin is a primary line of treatment while newer drugs such as SGLT-2 inhibitor and GLP-1 receptor agonist are secondary line of treatment options for these patients to prevent the development of CV disease.
Step 7 – Aspirin Use
For decades aspirin has been useful in individuals with established CV disease to decrease risk of future cardiac events such as a heart attack. However, there is an increased risk of bleeding associated with aspirin use. For healthy individuals without established CV disease who have a low CV risk profile the increased risk of bleeding with aspirin use outweighs the benefit of cardiovascular disease prevention. For this reason it is recommended that use of aspirin for primary prevention of CV disease should be reserved only for selected patients with a high CV risk profile. Use of aspirin should therefore be discussed with your physician prior to considering starting or stopping an aspirin regimen.
Conclusion – Putting it all together!
The 2019 ACC AHA Primary Prevention guideline1 focuses on a heart healthy lifestyle and focuses on a patient centered approach that emphasizes active engagement and discussion between patient and physician to determine the best customized approach and recommendations based on an individual’s CV risk profile.
There are several patient related resources such as:
- ACC Cardiosmart: https://www.cardiosmart.org/Heart-Conditions/Guidelines/Primary-Prevention-Heart-Disease
- American Heart Association: https://www.heart.org/en/health-topics/consumer-healthcare/patient-education-resources-for-healthcare-providers

References:
- WRITING COMMITTEE MEMBERS, Arnett DK, Blumenthal RS, Albert MA, Michos ED, Buroker AB, Miedema MD, Goldberger ZD, Muñoz D, Hahn EJ, Smith Jr SC, Himmelfarb CD, Virani SS, Khera A, Williams Sr KA, Lloyd-Jones D, Yeboah J, McEvoy JW, Ziaeian B, ACC/ AHA TASK FORCE MEMBERS, O’Gara PT, Beckman JA, Levine GN, Chair IP, Al-Khatib SM, Hlatky MA, Birtcher KK, Ikonomidis J, Cigarroa JE, Joglar JA, Deswal A, Mauri L, Fleisher LA, Piano MR, Gentile F, Riegel B, Goldberger ZD, Wijeysundera DN, 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease, Journal of the American College of Cardiology (2019), doi: https://doi.org/10.1016/j.jacc.2019.03.010.
- The Physical Activity Guidelines for Americans: THe HHS Roadmap for an Active Healthy Nation. Second Edition. ADM Brett P. Giroir, MD








 settings (#SneakerDay every day!?). Can we make it “OK” to stand for a bit when our tracking devices remind us that we’ve been sitting for an hour? Can we support activity with locker rooms at work? Better and more accessible training for healthcare workers on exercise prescription? More clarity on the roles and qualifications of fitness professionals? #AHA18 had a heart failure “Hackathon” this year to generate novel ideas– can we come up with some innovative ways to improve implementation of the cheapest, most effective treatment we have for poor health?
settings (#SneakerDay every day!?). Can we make it “OK” to stand for a bit when our tracking devices remind us that we’ve been sitting for an hour? Can we support activity with locker rooms at work? Better and more accessible training for healthcare workers on exercise prescription? More clarity on the roles and qualifications of fitness professionals? #AHA18 had a heart failure “Hackathon” this year to generate novel ideas– can we come up with some innovative ways to improve implementation of the cheapest, most effective treatment we have for poor health?