There has been an ongoing misconception of weight being a consequence of over-nutrition. The relationship between calorie intake versus calories spent continues to overshadow the biological forces that resist the maintenance of weight. Although scientists started to recognize obesity as a chronic disease in 1985, it was about 28 years later before the American Medical Association made the acknowledgement. The recognition of obesity being classified in the cluster of metabolic syndrome (MS) was a significant milestone in weight loss and primary health care.
Metabolic syndrome (MS) is defined as a homeostatic disturbance in the metabolic system characterized by visceral obesity, atherogenic dyslipidemia, hypertension, insulin resistance, and more recently, adipose tissue dysfunction. Increasing studies are exploring adipose tissue (AT) as an endocrine organ system encompassing physiological functions that assist in the regulation of weight, insulin sensitivity, inflammation, and vascular function. Matthews et al (opens in a new window) described the role of macrophages in the inflammatory response. Additionally, Dias et al (opens in a new window) expounded on the various inflammatory cytokines in AT that can potentially be modulated suggesting an anti-inflammatory role for statins. These reports have demonstrated a reduction in stress-induced inflammatory cytokines such as IL-6 and C-reactive protein as well as the upregulation of PPARγ, inhibition in ER stress, PA1 promoter activity through MAPKKK1 and to a lesser extent NFκB with the therapeutic use of statin drugs. There are conflicting data on the utilization of statins; however, their potential to induce the expression of PPAR and SRB1 in adipocytes can directly and inadvertently lower cholesterol and SRB1 stimulation. Generally, obesity has been controlled using pharmaceutical supplements; some examples include: Topiramate, Diethylpropion, Phentermine, and Lorcaserin. Among the medicinal weight therapies, Orlistat plays a direct role in digestion by inhibiting the absorption of dietary fat and subsequently body weight reduction. Orlistat inhibits diacylglycerol lipase (DAGL), the enzyme that catalyzes the hydrolysis of diacylglycerol leading to the liberation of free fatty acids and monoacylglycerol. This information is noteworthy due to the mechanistic pathways delineated in an article by Matthews and Lee (opens in a new window) (Figure) suggesting an important connection between the endocannabinoid ligand 2-arachidonylglycerol (2-AG) and oxidized low density lipoproteins (oxLDLs). This group and others have demonstrated DAGL and PLC-β are Ca2+ dependent enzymes that are important in the biosynthesis of 2-AG. However, during my time in Dr. Matthew Ross’s lab we found oxyradical fluxes and 2-AG generation had a positive correlation that lead to an antioxidant and anti-inflammatory effect associated with the 2-AG ligand. Thus, Orlistat combined with a low-calorie diet can have a synergetic effect of inhibiting fat absorption, reducing leptin concentration in plasma, CRP, IL-6 TNFα and inducing vascular protection.
In relation to food and nutrition, there are several articles that are related to the mechanistic action of the gut in relation to blood pressure including the role of gut microflora, oxidative stress, and lipid pathways that lead to metabolic changes. Being that my knowledge of nutrition is limited. I interviewed Tina Brown, FNP (opens in a new window) from Elite Health for expert advice.
I met Tina one morning on my way to campus. As I started my long walk down the sidewalk, I saw a sign across from a restaurant saying, “Weight Loss”. I thought to myself, “There is always a weight program somewhere. I’m in Memphis after all.” Memphis is known for their food, such as the Green Beetle that became popular back in 1939, the flavorful Curry-N-Jerk Caribbean cuisine, BB King BBQ Joint, the Redbird Field food court, and anything down Beale Street. Memphians are foodies and have the whole month of May dedicated to Blues and Barbeque! So, it comes as no surprise to see a “Weight Loss” facility in Memphis. Shelley White-Means, PhD (opens in a new window), University of Tennessee Health Science Center presented on, “Disparities in Breast Cancer Mortality: A Perfect Storm in Memphis.” I would like to modify that to say, “Disparities in CVD mortality: A Perfect Storm in Memphis” due to the culture and prevalence of food, as well as the activities surrounded by an abundance of great barbeque.
I spoke with Tina via phone in addition to a face-to-face interview. To give some background as to why nutrition is an important second step in one’s health journey, it is important to understand that one in three Americans are diagnosed with a metabolic dysfunction consistent with cardiovascular disease, such as hypertension, diabetes, renal dysfunction, or obesity.
The interview went as follows:
Q1. What are your qualifications?
A. I attended Nursing school at University of Memphis (@UofM) as an adult learner receiving a Bachelor of Science in Nursing. After working for several years as a nurse, first doing rotations and finally settling in the medical surgical unit I returned to UofM to specialize.
Q2. Are you aware of any nutritional requirements for a patient that has cardiovascular disease namely, hypertension?
A. I was watching an infomercial about L-Arginine and how it helps with cleaning the vascular system and vasodilation. After watching for several minutes, I realized it was an infomercial, but it was good information and research. I don’t recall the author.
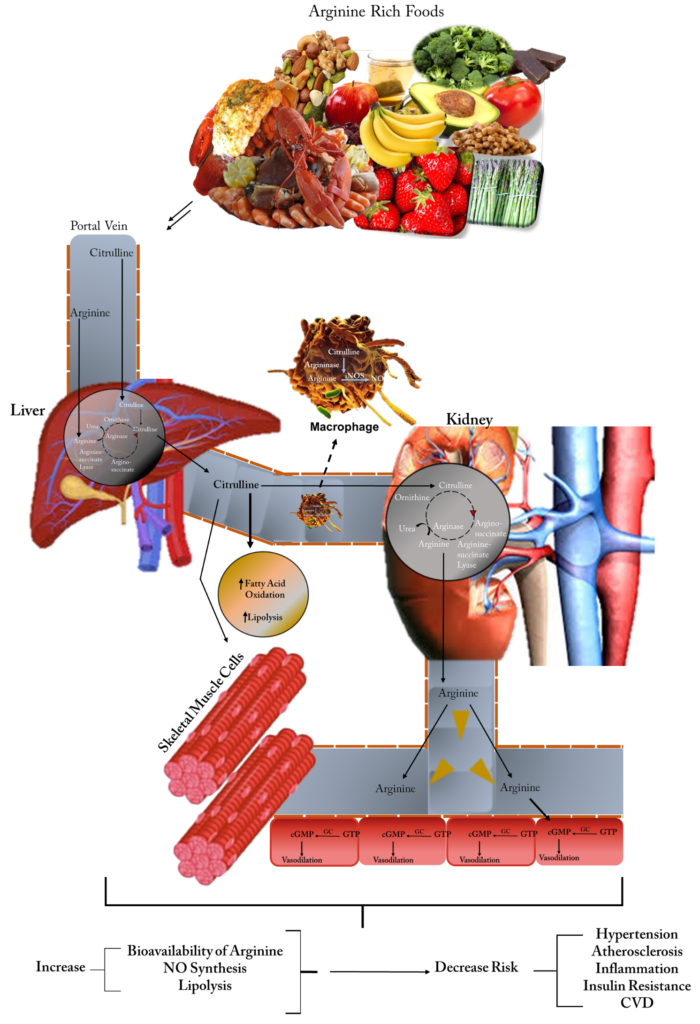
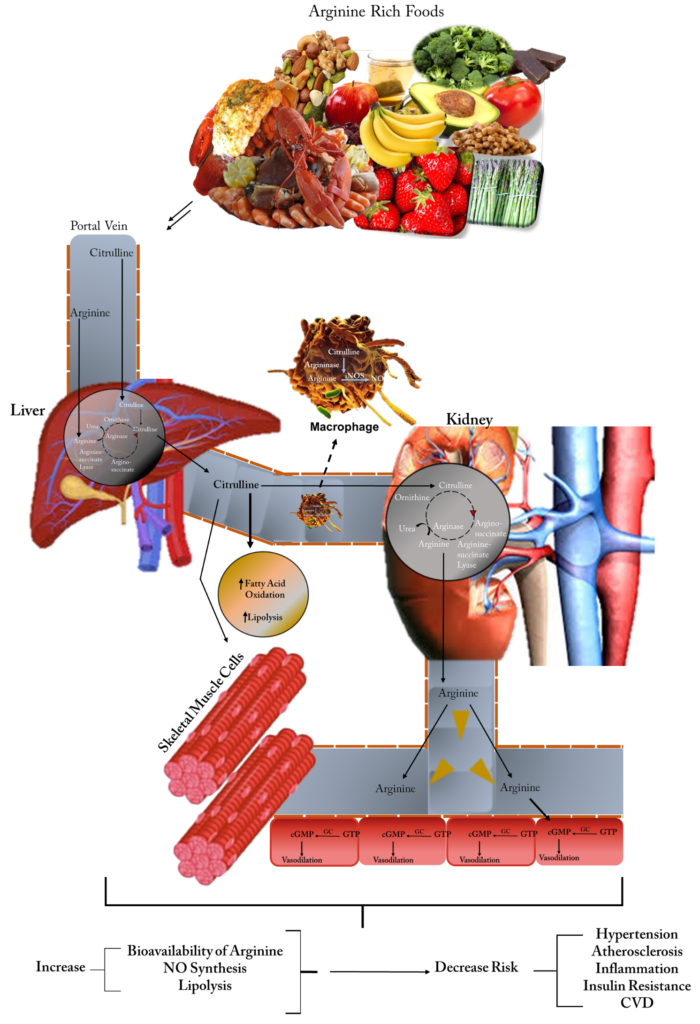
Note: Upon looking for the information, I was not able to find the exact infomercial that Tina was referring; however, I did find information on L-arginine’s effect on the vascular system. Arginine is the precursor for nitric oxide (NO) in endothelial nitric oxide (eNOS), since eNOS is necessary for gas exchange and the regulation of various biological functions it is reasonable that L-arginine can play a role in maintaining vascular homeostasis. Allerton et al (opens in a new window) (Figure) compared in a review the use of L-arginine with citrulline supplementation to determine whether there were any significant changes in cardiometabolic health. Patients with elevated blood pressure has been reported to display labs with reduced NO bioavailability and subsequent vasoconstriction. Incorporating L-arginine (and l-citrulline) into the diet can potentially indirectly or directly increase vasodilation by increasing eNOS expression and NO production thereby its bioavailability leading to reduced blood pressure.
Q3. What advice will you give a patient regarding these diagnoses?
A. Eating a low carbohydrate diet. Choosing the good carbs such as eliminating white bread and sugars.
Note: In a randomized clinical trial, Dr. Christopher Gardner et al (opens in a new window). evaluated the effects of low-fat (HLF) versus low-carbohydrate (HLC) healthy diets to determine whether there were any genotypic alterations in regard to weight loss that were effected by either of the dietary patterns. The HLF or HLC diets had no statistical significant in weight loss by genotype, insulin interactions. These data and others suggest that eating a low carb diet can be beneficial in weight loss, but in addition to other healthy lifestyle changes. Especially in light of statin therapy assist in reduction in fat absorption.
B. Combining the ketogenic diet (high protein, high fat) and paleo (organic) diets together can work as a sustainable diet that will allow one to get all the nutrients the body need to work properly. The keto diet done alone is not as healthy:
- Ketogenic diet is a plan that consist of minimizing carbohydrate intake while maximizing fats to force the body to use fat as its form of energy for expenditure. Generally, this mechanism translates to calories being consumed from 60-75% fat, 15-30% protein, and 5-10% carbohydrates. On average it takes about 2-7 days for the body to go into ketosis on this meal plan.
- Paleolithic times was a period when certain food stuffers were not available, thus the paleo diet is a nutritional approach that is focused on eating unprocessed foods based on those guidelines. The primary backbone of it is to only consume food that would have been available before the industrial agriculture, domestication of animals, and modern food processing.
Note: There is a vast amount of research indicating that branched chain amino acids (BCAA) are linked to diabetes, and this is showing an increasing trend over the past decade. In an Editorial in the Journal of Diabetes (opens in a new window), Bloomgarden described a Young Finn’s Study suggesting phenylalanine and tyrosine, aromatic amino acids are linked to insulin resistance in men and obesity my track more strongly in the presence of BCAA. In addition to BCAA leading to increased risk of MS: obesity CVD, dyslipidemia, and hypertension; medium-and long-chain acylcarnitine’s, the metabolic byproducts of mitochondrial catabolism of BCAA, plays a role in insulin resistance.
C. Know that vitamins are being taken and do not just listen to what you are hearing. If you are healthy, you will lose weight as a side effect if weight loss is necessary. Making lifestyle changes that will result in small gains will generate the momentum needed to be successful in moving forward in sustaining the lifestyle. Once a person sees results, compliance becomes easy.
Note: Dalia Gaddis, PhD and Wei Ling Lau, MD also gave some insightful information in their blogs on these topics such as: “Weight Loss and Exercise: A Remedy For A Better Functioning HDL”, “Can Increasing HDL Reduce Heart Disease? An Issue of Constant Debate!”, “Natural Supplements Can Be A Pain in The Kidneys” and “If you give a patient calcium…” respectively.
D. Increasing physical activity is important. One must get the heart rate up and maintain the increased heart rate for short intervals (Note: it is recommended to get heart rate up for ~30 minutes 3 days per week). Doing simple things make a big difference such as standing up and moving around. Incorporate things that will make the muscles work rather than just sitting or standing stationary. For example, there are now the balance boards to stand on at the standing desk, or a body ball to sit on at a sitting desk.
Note: “Therapeutic elevation of HDL-Cholesterol to prevent atherosclerosis and coronary heart disease” Pharmacology and Therapeutics 2006 (opens in a new window); 111(3):893-908. The study delineated that HDLs play a role in cholesterol transport. However, Ross et al (opens in a new window) suggested only free cholesterol is effluxed from macrophages via ABCA1 transporters. It has also been reported that macrophage cholesterol exchange can be modulated by toxins in the body by down regulation of CD36 and SR-A protein expression.
Q4. How will you advise a patient suffering with CVD symptoms on improving their vascular health from a nutrition standpoint?
A. Get weight under control. Determine the underlying reason/condition behind the weight gain/vascular injury. Determine whether there is a metabolic disorder, rule out any hormonal deficiencies such as thyroid or testosterone, vitamin levels
B. Reduce any inflammation if necessary by potentially using a low dose pharmaceutical regimen until the patient lose weight or get hypertension under control. Especially if it is acute rather than chronic.
Q5. Any overall/general nutritional guidelines you would suggest for a patient with hypertension to consider modifying?
A. Meal preparation is the best option. By planning meals, one can look ahead at the menu and make good choices about what is being prepared. Even going to the grocery store, shopping the perimeter will generally give the healthier options.
B. Avoid eating out. When meals are prepared at home everything that goes in the meal can be a healthy option without any cheats. When eating out, one never knows whether there are cheats such as saturated fats or salts
C. Limit sodium intake
D. Have healthy snacks readily available. This will help cut cravings and avoid picking up unhealthy sugary snacks due to the feeling of needing to eat quickly. If a person has the personality that they must eat all the time, it will be hard if not impossible to change, having healthy snacks on hand such as fermented snacks (pickles or sauerkraut) or dehydrated fruit and veggies is better than forcing them to change and these snacks assist in weight loss.
Q6. How important is reporting back to the physician/counselor?
A. Very important, accountability helps with compliance. It is also a trust issue; the medical professional wants them to want to come back. The patient needs to be able to ask questions and discuss any changes in treatment. If a patient starts to lose or gain weight their medicine may need to change thus making it necessary to visit the physician/counselor regularly. It is also a good idea to have a fitness buddy to hold each other accountable.
It is important to not only visit the doctor but also to ask questions about your health. Take the challenge to be the best you that you can be.
Upcoming posts:
• Fitness coaching
• Mental coaching
Leave a comment or tweet @AnberithaT and @AHAMeetings if you have questions or are interested in something else specifically.
Follow me and @American_Heart for more #HeartSmart information.

Anberitha Matthews, PhD is a Postdoctoral Fellow at the University of Tennessee Health Science Center in Memphis TN. She is living a dream by researching vascular injury as it pertains to oxidative stress, volunteers with the Mississippi State University Alumni Association, serves as Chapter President and does consulting work with regard to scientific editing.
 Unsurprisingly, almost all of my patients I’ve seen over the past year have fallen victim to this, with good reason. They are protecting their health by avoiding exposure to COVID-19 but at the same time are unconsciously neglecting their health by not having the means or green light to engage in healthy behaviors such as going to the gym, walking in public spaces, and engaging in aerobic exercise and strength training. Our current restrictive environment combined with more time at home to eat and indulge is a fail-proof setup for adding on these harmful extra pounds.
Unsurprisingly, almost all of my patients I’ve seen over the past year have fallen victim to this, with good reason. They are protecting their health by avoiding exposure to COVID-19 but at the same time are unconsciously neglecting their health by not having the means or green light to engage in healthy behaviors such as going to the gym, walking in public spaces, and engaging in aerobic exercise and strength training. Our current restrictive environment combined with more time at home to eat and indulge is a fail-proof setup for adding on these harmful extra pounds. For many of us, we understand what we should eat to become healthier, however, that does not mean we will actually follow this rationale to maintain a heart-healthy diet, especially during a pandemic when most of our day is spent sedentary in isolation at home. Despite having a master’s degree in Nutrition as part of my training, I can admit that I have invariably fell victim to the vices of food comfort at home. I was eating a lot of baked desserts after dinner but recently decided to replace this habit with a cup of hot chocolate made with soy milk and sugarless cocoa powder.
For many of us, we understand what we should eat to become healthier, however, that does not mean we will actually follow this rationale to maintain a heart-healthy diet, especially during a pandemic when most of our day is spent sedentary in isolation at home. Despite having a master’s degree in Nutrition as part of my training, I can admit that I have invariably fell victim to the vices of food comfort at home. I was eating a lot of baked desserts after dinner but recently decided to replace this habit with a cup of hot chocolate made with soy milk and sugarless cocoa powder.