Attending AHA19 Online From Anaheim, CA
 I have gone back and forth with attending the American Heart Association (AHA) Scientific Sessions online in 2017 (AHA17), to onsite (AHA18), and this year (AHA19) I attended online again. There was absolutely no comparison between attending AHA18 to the online versions! I was the first to say that going to conference is overwhelming because there is so much to see and so many people to meet. I have since come to appreciate the benefits to attending meetings onsite. Generally, I stay within my session [Atherosclerosis, Thrombosis, Vascular Biology (ATVB) or Hypertension (HTN)]. Attending online gives some limitations, such as being at home, work, or traveling, there is a time restraint as well as multiple distractions. I experienced them all! I was traveling to a conference that conflicted with AHA19, thus the distractions of traveling and keeping up with my meeting responsibilities was a lot to juggle. Once I was home, there was everything that goes along with getting settled back into the routine of things that gave me a distraction. This year was a beast of responsibilities, but before I discourage you from attending a meeting online, let me share some benefits and things that I enjoyed about having the flexibility of being online rather than onsite.
I have gone back and forth with attending the American Heart Association (AHA) Scientific Sessions online in 2017 (AHA17), to onsite (AHA18), and this year (AHA19) I attended online again. There was absolutely no comparison between attending AHA18 to the online versions! I was the first to say that going to conference is overwhelming because there is so much to see and so many people to meet. I have since come to appreciate the benefits to attending meetings onsite. Generally, I stay within my session [Atherosclerosis, Thrombosis, Vascular Biology (ATVB) or Hypertension (HTN)]. Attending online gives some limitations, such as being at home, work, or traveling, there is a time restraint as well as multiple distractions. I experienced them all! I was traveling to a conference that conflicted with AHA19, thus the distractions of traveling and keeping up with my meeting responsibilities was a lot to juggle. Once I was home, there was everything that goes along with getting settled back into the routine of things that gave me a distraction. This year was a beast of responsibilities, but before I discourage you from attending a meeting online, let me share some benefits and things that I enjoyed about having the flexibility of being online rather than onsite.
With all the distractions I experienced viewing AHA19 online, the main benefit was that I was able to watch sessions at my own pace as well as read the transcripts while the speaker was talking. In previous years I did not use that function; this year, I used it for almost all sessions, and it was wonderful. To be able to take screenshots of the talk and look things up later was the best tool in my toolbox. Additionally, there was a textbox that allowed viewers to ask questions to the speaker without standing in long lines and potentially not getting a response. That has happened to me more times than not because, as chance would have it, the best speakers and researchers show up to AHA meetings. These are the opportunities to get the best guidance regarding research methodology, mentoring, clinical expertise, and networking with some of the best in every discipline from around the globe.
I had the privilege of sitting in on several topics that sparked my interest. For example:
- Update in Clinical Lipidology – Aspirin: Who Needs it Anymore? Discussing what markers should be considered with prescribing aspirin; role of and how to interpret the stenosis score; and considerations of patients with diabetes, family history of nonclassified plaque
- Clinical Trials—ASPREE (JJ Mcneil, NEJM 2018; MATCH); ISAR REACT 5 Trial; and GLOBAL LEADERS)
Share some of your favorite parts of AHA19 with me in the comments or follow me on Twitter (@AnberithaT); also @ahameetings and @ATVBCouncil. Let’s keep this conversation going. Did you attend online or onsite?
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.
 We are faced with a number of changes in our lives. The old saying, “life happens” generally means take the changes as they come and keep it moving. The human body is not equipped to distinguish between distress and eustress. Amazing life changes happens such as getting acknowledged for an accomplishment, passing the preliminary exams for a PhD program, getting the job of your dreams, or even getting the funding you have worked so hard to apply for consideration. Contrarily, changes that can be viewed as less than optimal such as being passed over for a promotion, losing the sole source of your family’s income, death of dreams, and rejection are all sources of stress. Good or bad, these events affect hypertensive rates potentially leading to a more serious chronic illness such as heart attacks, strokes, or even metabolic disease.
We are faced with a number of changes in our lives. The old saying, “life happens” generally means take the changes as they come and keep it moving. The human body is not equipped to distinguish between distress and eustress. Amazing life changes happens such as getting acknowledged for an accomplishment, passing the preliminary exams for a PhD program, getting the job of your dreams, or even getting the funding you have worked so hard to apply for consideration. Contrarily, changes that can be viewed as less than optimal such as being passed over for a promotion, losing the sole source of your family’s income, death of dreams, and rejection are all sources of stress. Good or bad, these events affect hypertensive rates potentially leading to a more serious chronic illness such as heart attacks, strokes, or even metabolic disease. Dr. Karen Griffin, who presented a seminar in April 2019 at the University of Tennessee Health Science Center (UTHSC) Department of Physiology, has carried the FAHA designation for several years, but now serves as Chair of the
Dr. Karen Griffin, who presented a seminar in April 2019 at the University of Tennessee Health Science Center (UTHSC) Department of Physiology, has carried the FAHA designation for several years, but now serves as Chair of the 
 The Experimental Biology conference is here again! This year we donned on the wonderful city of Orlando, FL (April 6-10, 2019) where we fill the air with all topics physiology. Generally, we only look at the research portion of meetings/science, but what about the future generations that are to come up after us? The American Physiological Society has implemented initiatives to address that question. I spend my day following the PhUN (Understanding Physiology) sessions where undergraduate students presented their summer research projects and K-12 teachers learned how to incorporate physiology in the classroom.
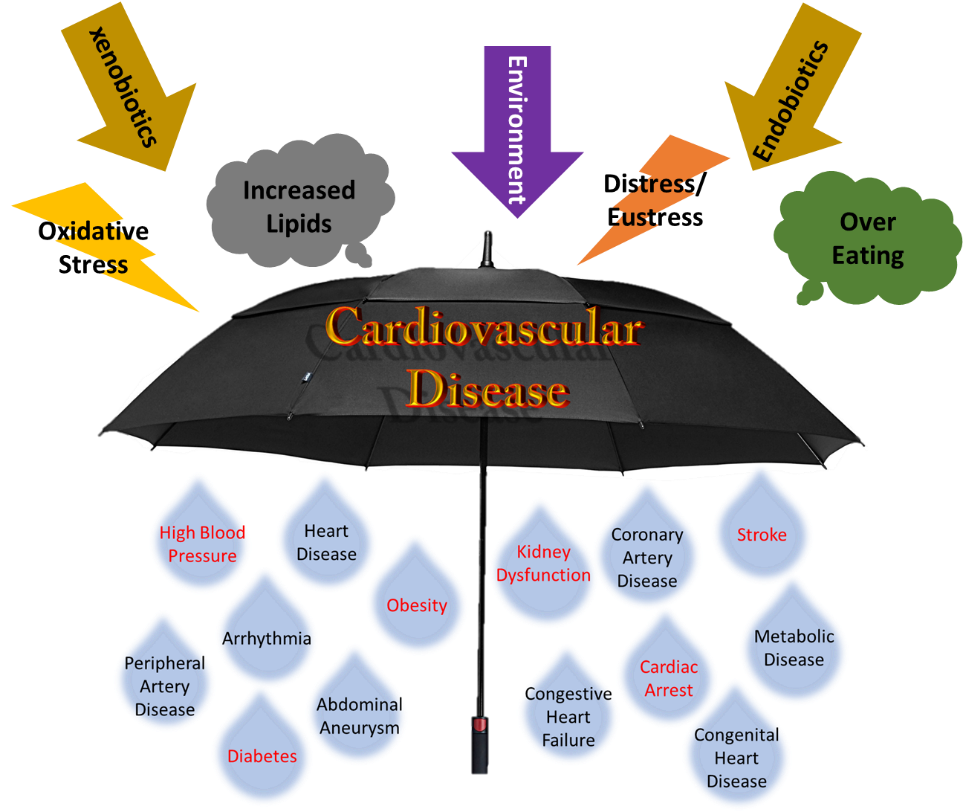
The Experimental Biology conference is here again! This year we donned on the wonderful city of Orlando, FL (April 6-10, 2019) where we fill the air with all topics physiology. Generally, we only look at the research portion of meetings/science, but what about the future generations that are to come up after us? The American Physiological Society has implemented initiatives to address that question. I spend my day following the PhUN (Understanding Physiology) sessions where undergraduate students presented their summer research projects and K-12 teachers learned how to incorporate physiology in the classroom. As an Outreach Fellowship recipient from the APS and a vascular scientist, I participated in PhUN week at Sale Elementary School in Columbus. Being that PhUN week was focused on cardiovascular disease, I took a box of lab supplies out to the school to teach the students lab safety, how to collect primary cells, prepare them for slides, and view them under the microscope. I spent the last two days teaching how we use their classroom math in protocol formulation and subsequently writing techniques to summarize the findings. As serendipity would have it, the students were on a section that were easily translatable to what I prepared as talking points.
As an Outreach Fellowship recipient from the APS and a vascular scientist, I participated in PhUN week at Sale Elementary School in Columbus. Being that PhUN week was focused on cardiovascular disease, I took a box of lab supplies out to the school to teach the students lab safety, how to collect primary cells, prepare them for slides, and view them under the microscope. I spent the last two days teaching how we use their classroom math in protocol formulation and subsequently writing techniques to summarize the findings. As serendipity would have it, the students were on a section that were easily translatable to what I prepared as talking points. Getting to Hawaii was quite the event! I underestimated the flight and how I would feel with such time zone changes. However, the International Stroke Conference 2019 (#ISC19) was worth all the efforts. The meeting objectives were sufficiently described in the program book and
Getting to Hawaii was quite the event! I underestimated the flight and how I would feel with such time zone changes. However, the International Stroke Conference 2019 (#ISC19) was worth all the efforts. The meeting objectives were sufficiently described in the program book and