Role of Curcumin on Inflammation
There has recently been a craze about using turmeric for a number of health-related issues. Are these claims valid? What is turmeric anyway? I mean, where did it come from and what is the mechanism of action if this root does indeed work for improving health? I intend to reveal here whether jumping on yellow wagon is worth the hype.
Being a rhizomatous, herbaceous perennial from the ginger family, this plant is native to the Indian subcontinent and Southeast Asia. To preserve these roots after harvest, the rhizomes are boiled, dried and ground into powder that can be used for cooking, coloring, and flavoring in many dishes such as curries. It is often used in Ayurvedic medicine because of the curcumin constituents that are thought to be therapeutic. However, curcumin makes up approximately 3% (with an average of 1.5%) of turmeric powder commercially sold including curcumin, demethoxycurcumin, and bisdemethoxycurcumin. Interesting!!! What about the essential oils, you may ask? There are about 34 oils, including tumerone, germacrone (antiviral isolate), atlantone, and zingiberene (the monocyclic sesquiterpene component of ginger comprising ~30% of the essential oils).
Traditionally, turmeric was used in traditional Siddha or Ayurveda medicine, generally place on the skin or adorned the body. For example, during the Haldi ceremony, Gaye holud (yellow on the body), turmeric is used in weddings. In Tamil Nadu and Andhra Pradesh, it is strung into a necklace, or in Marathi the tubers are tied by the couples to their wrists. However, because it is sold by weight, it is commonly adulterated by the addition of toxic powders such as lead oxide, changing the color from its native golden yellow to an orange-red color. Additionally, a compound known as acid yellow 36 is added for use in food products but is deemed illegal in some countries. Does this now make you want to read the label of the turmeric in your spice cabinet? However, in traditional medicine, curcumin has been used to alleviate respiratory conditions, anorexia, coryza, cough, and hepatic diseases.
Research is now supporting the medicinal uses for turmeric’s active ingredient, curcumin, because it has been demonstrated to reduce pro-inflammatory-induced chronic illnesses including cardiovascular, metabolic, pulmonary, auto immune and malignant diseases (Prasad et al). This group went on to suggest that inhibition of transcription factors nuclear factor-kappaB (NF-κB), Wnt/beta-catenin, and activates peroxisome proliferator-activated receptor-gamma and Nrf2 cell signaling pathways. Modulating these activities can potentially lead to downregulation of adipokines and upregulation of adiponectin and other gene products. Curcumin has also been shown to modulate not only cell survival proteins and inflammatory components on a biological level, but it has also been linked to histone acetylase, deacetylase, protein kinases and reductases, and glyoxalase I, as well as DNA, RNA, and metal ions. Needless to say, these are a vast number of pathways being acted upon by this compound.
A recent article by Dai et al suggest curcumin plays a role in alleviating collagen-induced inflammation by targeting the mTOR pathway. Although this study is focused on rheumatoid arthritis, the inflammatory markers that were explored play a vital role in vascular inflammation such as chemokines, cathepsin, matrix matalloproteinases, TNF-α, and IL-1 to breakdown the extracellular matrix and ultimately lead to vascular remodeling. Curcumin is considerably cheap and easily available, making it attractive to use in inflammation studies. Rapamycin (mTOR) role in cellular proliferation, differentiation, and apoptosis makes it an important player in cellular regulation. Using Wistar rats as their model, Dai et al suggest curcumin can potentially inhibit the mTOR pathway under collagen-induced inflammatory conditions when compared to the control group. Additionally, this group demonstrated a reduction in inflammatory cell infiltration in the treatment group alleviating the hyperplasia with curcumin therapy.
Promising results were demonstrated by Xiao et al with hemeoxygenase-1 (HO-1) with cytoprotective effects under some pathological conditions. This group used New Zealand white rabbits that were fed curcumin for four weeks. Once the acute vascular inflammation was induced, there was an increase in serum bilirubin and vascular, liver, and spleen HO-1 mRNA levels with curcumin treatment compared to control, as well as a decrease in vascular inflammation. Furthermore, with HO inhibition or HO-1 siRNA knock down, there was an amelioration of carotid artery HO-1, impeding vascular inflammation. Xiao et al went on to report treatment of human artery endothelial cells with curcumin lead to the activation of the Nrf2 and p38 MAPK signaling pathways.
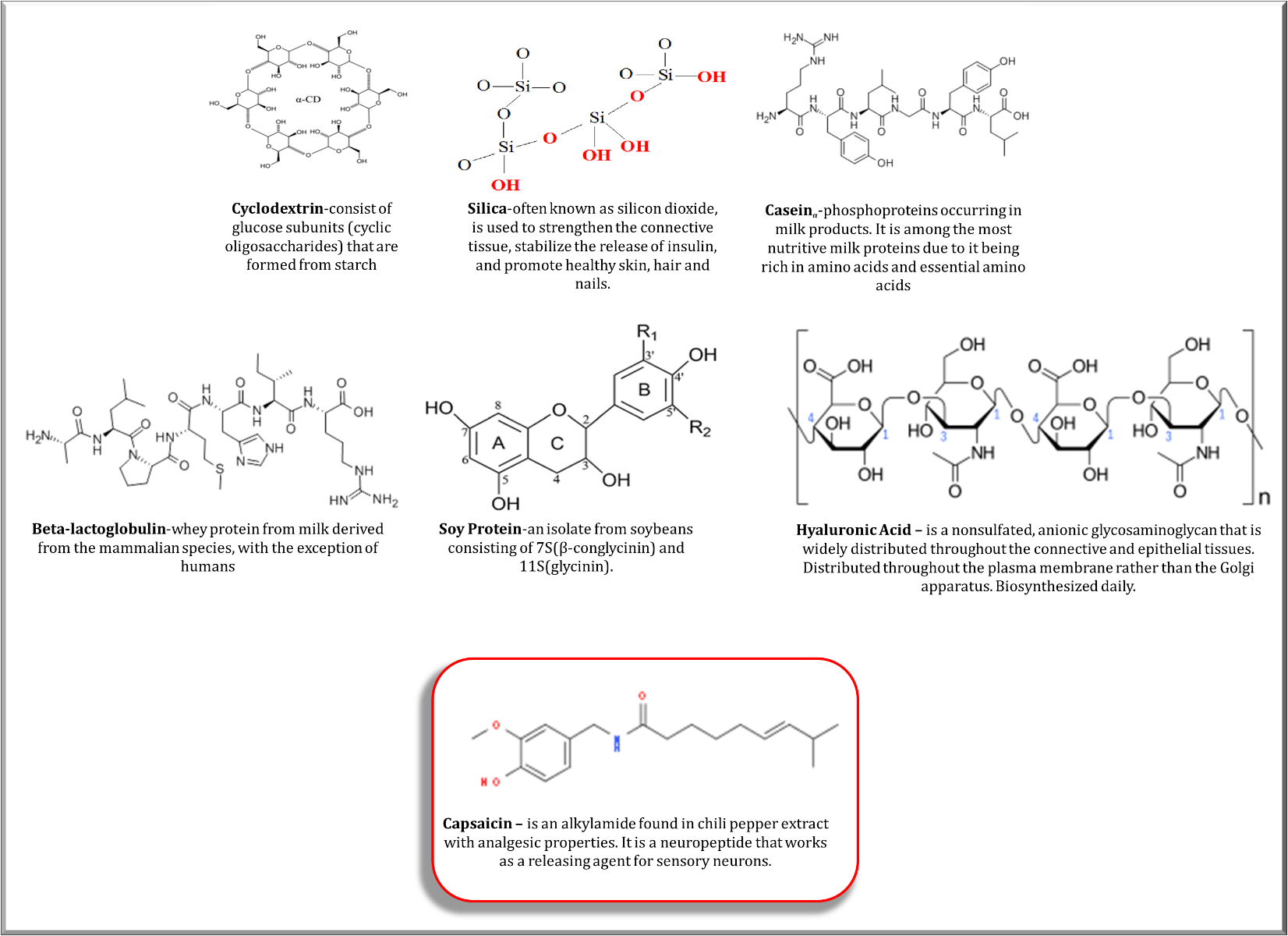
Ultimately, the active compound in turmeric, curcumin, has been shown to contribute to the reduction of vascular inflammation in addition to rheumatoid arthritis-induced inflammation by decreasing the proinflammatory cytokines and chemokines. Additionally, antioxidant response elements are responsive in the presence of curcumin. The thing to remember here is, with all the positive results, curcumin is not readily bioavailable. To get a therapeutic amount, it should be formulated with delivery compounds such as capsaicin or hyaluronic acid (see image). Furthermore, the dose that is necessary to have an effect may be higher than the amount delivered if it is not correctly monitored. For example, it takes up to 90 mg orally to attenuate oxidative stress following a downhill run according to Kawanishi et al. This reduction was observed due to the increase in the blood’s antioxidant capabilities that utilize the TNF, cyclooxygenase-2, and iNOS to initiate anti-inflammatory mechanisms.
So the question, is it a good idea to jump on the yellow band wagon? Yes. However, some things to keep in mind is to read the labels to be sure the turmeric is pure or try to purchase the root in its native form and dry it to the powder at home. Do your research to make sure you are consuming enough to get the benefits from the product. Make sure you are mixing it with the right compounds. I have been utilizing turmeric for years before this band wagon came along, and I will continue to purchase turmeric roots from the farmer’s market and make powder by drying it out in a low temperature oven overnight (get to the powder by blending in the Ninja Blender). I do not think I will use the diatomaceous earth (silica) that was suggested in one of the recipes I saw online.
If you are interested in recipes using turmeric, there are a lot on @dashdiet1 www.AHA.org. I also post on my twitter.
Remember to follow me on Twitter @AnberithaT where I will keep you posted on #AHAMeetingsReports @AHA_Meetings and #VascularScience. See you in Hawaii for #ISC2019!
 Imagine having an annoying pain that you thought was just a pulled muscle. No, I am not referencing that episode of The Resident, a medical drama prime time series aired by Fox, where a young immigrant was having pains in her side and it ended up being a rare cancer. However, I am referring to a real-life hero story about Roxanne (an organ recipient) and Michael (an organ donor). Roxanne had complaints of side pain for about a week, but she continued to work because she thought it was a pulled muscle. She tolerated the pain for about six weeks before she arrived at the emergency room (ER) where she was diagnosed with cardiovascular disease (CVD). She was immediately taken into cardiac care, underwent extensive diagnostic test, and her medical team concluded they could not give her the required treatment locally. Roxanne was transferred to the Cardiac Care unit in Bronx, New York where she was admitted to the hospital for nine days of extensive medical consultations. Upon receiving the diagnostic results, her primary physician approached her with both good news and bad. The bad news was that her heart had started to fail; the good news was she was in a state of stable instability. Roxanne was placed on list to receive a heart transplant as Stat 2.
Imagine having an annoying pain that you thought was just a pulled muscle. No, I am not referencing that episode of The Resident, a medical drama prime time series aired by Fox, where a young immigrant was having pains in her side and it ended up being a rare cancer. However, I am referring to a real-life hero story about Roxanne (an organ recipient) and Michael (an organ donor). Roxanne had complaints of side pain for about a week, but she continued to work because she thought it was a pulled muscle. She tolerated the pain for about six weeks before she arrived at the emergency room (ER) where she was diagnosed with cardiovascular disease (CVD). She was immediately taken into cardiac care, underwent extensive diagnostic test, and her medical team concluded they could not give her the required treatment locally. Roxanne was transferred to the Cardiac Care unit in Bronx, New York where she was admitted to the hospital for nine days of extensive medical consultations. Upon receiving the diagnostic results, her primary physician approached her with both good news and bad. The bad news was that her heart had started to fail; the good news was she was in a state of stable instability. Roxanne was placed on list to receive a heart transplant as Stat 2. Roxanne has changed her activity of daily living to accommodate the dietary habits suggested by her nutritionist in addition to referencing a book she received outlining the things that she could and could not continue to remain healthy. She was adamant about following the instructions that were given because she did not want to risk damaging her new heart. She is now a self-proclaimed foodie although she had no interest in food or cooking to the extent she has developed. She has taken cooking classes and learned more details about mixing spices. Roxanne regularly attends conferences and deliver seminars to assist in her goal of encouraging people become organ donors. Roxanne has become an advocate for people that cannot advocate for themselves. This is an example that all can admire. Michael, real-life superhero, lives on though Roxanne as she goes on a mission to change people’s outlook on organ donations.
Roxanne has changed her activity of daily living to accommodate the dietary habits suggested by her nutritionist in addition to referencing a book she received outlining the things that she could and could not continue to remain healthy. She was adamant about following the instructions that were given because she did not want to risk damaging her new heart. She is now a self-proclaimed foodie although she had no interest in food or cooking to the extent she has developed. She has taken cooking classes and learned more details about mixing spices. Roxanne regularly attends conferences and deliver seminars to assist in her goal of encouraging people become organ donors. Roxanne has become an advocate for people that cannot advocate for themselves. This is an example that all can admire. Michael, real-life superhero, lives on though Roxanne as she goes on a mission to change people’s outlook on organ donations.

 As serendipity will have it, I met a summer student while I was having lunch in the common break room (which I never do because who has time for lunch?). This student was studying
As serendipity will have it, I met a summer student while I was having lunch in the common break room (which I never do because who has time for lunch?). This student was studying  The months of March and April were filled with a whirlwind of conferences. I had the pleasure of traveling to several meetings across the U.S. including the
The months of March and April were filled with a whirlwind of conferences. I had the pleasure of traveling to several meetings across the U.S. including the 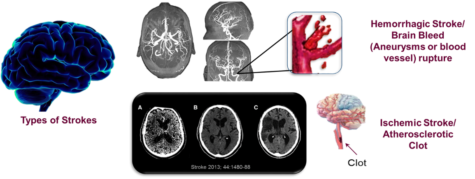 It has been well accepted that atherosclerosis is the result of chronic inflammation. I have spent several years exploring the role endocannabinoids, lipid-based neurotransmitters that bind to receptors that are expressed throughout the peripheral and central nervous system, play in decreasing oxyradical derived inflammation. Under normal conditions, lipids are metabolized and excreted from the body. It is my belief we have an endogenous mechanism that maintains balance within the vascular system that protects our arteries from becoming damaged; however, in the event of an injury the immune system is activated leading to cardiovascular dysfunction.
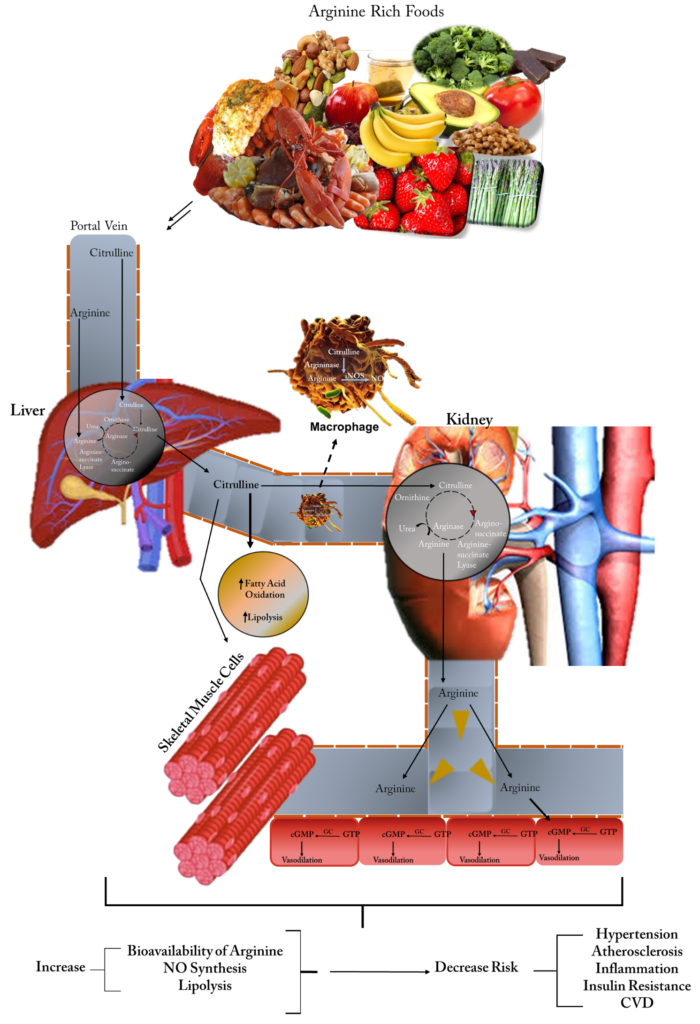
It has been well accepted that atherosclerosis is the result of chronic inflammation. I have spent several years exploring the role endocannabinoids, lipid-based neurotransmitters that bind to receptors that are expressed throughout the peripheral and central nervous system, play in decreasing oxyradical derived inflammation. Under normal conditions, lipids are metabolized and excreted from the body. It is my belief we have an endogenous mechanism that maintains balance within the vascular system that protects our arteries from becoming damaged; however, in the event of an injury the immune system is activated leading to cardiovascular dysfunction.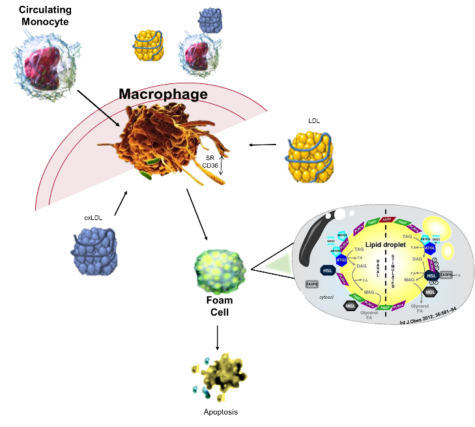 All strokes are not alike, they include ischemic, hemorrhagic, and transient ischemic attacks (TIA). Although older persons are thought to be the primary risk group for strokes, children and fetus can potentially be included in the risk population. The most common type is ischemic stroke caused by clots occluding the blood flow to the brain. The clots can be from congenital heart defects, sickle cell disease, and trauma that injures a large artery; however, they can also be a consequence of high cholesterol, oxLDL, and blood clots as well as
All strokes are not alike, they include ischemic, hemorrhagic, and transient ischemic attacks (TIA). Although older persons are thought to be the primary risk group for strokes, children and fetus can potentially be included in the risk population. The most common type is ischemic stroke caused by clots occluding the blood flow to the brain. The clots can be from congenital heart defects, sickle cell disease, and trauma that injures a large artery; however, they can also be a consequence of high cholesterol, oxLDL, and blood clots as well as