Joint Hypertension 2018 Scientific Sessions – You Should Have Been There

Just as promised, the Joint Hypertension 2018 Scientific Sessions (Hypertension18) was indeed among the most impactful meetings one could have attended. Council on Hypertension Scientific Sessions Planning Committee Vice Chair Dr. Karen Griffin, FAHA was accurate in her statement that it would be “the premier scientific meeting.” There were experts from all parts of the world covering more cardiovascular topics that I think my fingers could not keep up with in note taking, and each session was more informative than the next with up-to-date information on hypertension.
During the President’s Welcome Address, Dr. Ivor Benjamin, FAHA foreshadowed what was to be expected during the meeting. He gave general overviews of the hypertension guidelines, what the changes mean to clinicians and researchers, as well as the role AHA will play in helping drive those changes forward. His welcome was a great introduction to the ‘Recent Advances in Hypertension’ Session chaired by Drs. Joey Granger from the University of Mississippi Medical Center and John Bisognano from University of Rochester Medical Center. This session covered the new guidelines, implementation, and basic research advances of clinical hypertension moving forward by Drs Basile, Egan, Oparil, and Ellison. The whirlwind of information was just the icebreaker! During the refreshment break and exhibits, I met a number of “Rockstars” including clinicians and researchers from University of Alabama Birmingham, Drs. David and Jennifer Pollock and AHA Early Career blogger Tanja Dudenbostel. Additionally, this was the only time I spent visiting with vendors. Among them, Hulu explained the importance of calibrating automatic blood pressure machines. Historically blood pressure was taken with a manual sphygmomanometer and a technician listening for ausculatory sounds via a stethoscope, but now it is all automated. Generally one machine is used for all patients. This technology forces us to question the accuracy of the readings of the machines. Are they calibrated? Should the BP be taken radially or at the wrist? Should the machine be changed throughout the day? There was Aegis representatives sharing information about products to assist medical professionals determine patient compliance to therapy and toxicology testing equipment. During these conversations, it was surprising to discover some of the rationales behind why people would opt to not take medicine as prescribed.
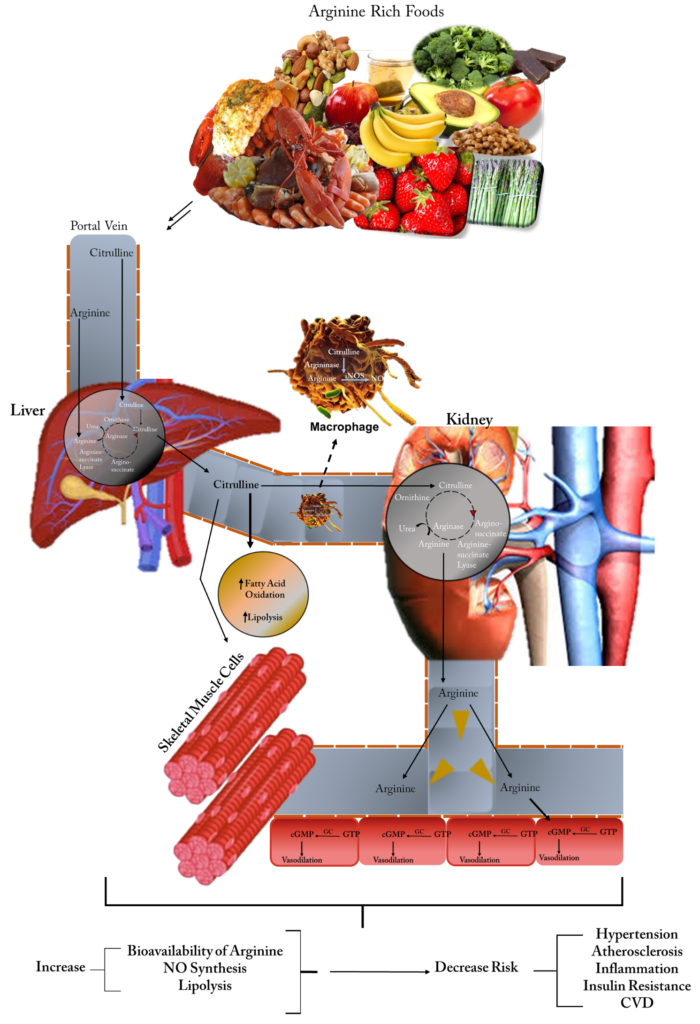
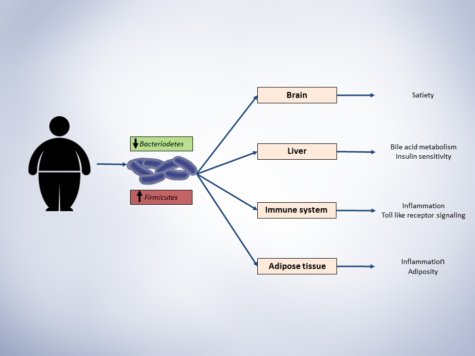
With my research being focused on oxidative stress-induced vascular injury and since I have become increasingly more interested in health and wellness, I took particular interest in the session focused on “Lifestyle Modifications and Impact on BP” chaired by the Associate Editor of Hypertension, David Harrison, MD, FACC, FAHA, “Recent Advances Obesity and Cardiovascular Disease” chaired by the consulting Editor of Hypertension Suzann Oparil, MD, FAHA, and “Obesity, Diabetes, and Metabolic Syndrome” chaired by Drs. Kamal Rahmouni and Carmen De Miguel. During these sessions, it was not surprising that regular exercise reduced vascular stiffness, but what was noteworthy was that weight training contributes to atherosclerosis. Additionally, the sympathetic nervous system seems to be important in glomerular filtration. Dr. Elizabeth Lambert delivered an intriguing talk about how diet and exercise can significantly decrease metabolic syndrome in middle aged obese individuals, which is consistent with a recent study (Hypertension18 Meeting Report P388) that suggests lifestyle changes can reduce hypertension in both men and women. Further, the study suggests that following the DASH diet, exercising, and weight management over a course of 16 weeks were contributing factors in reducing BP in test subjects. We all know anti-hypertensives work in reducing BP. Lifestyle changes should be the first line of defense in evading hypertension and getting it under control at the onset, according to the American Heart Association/American College of Cardiology Hypertension Guidelines. We have all heard that we have to get out there and get moving. Choosing the right exercise is just as important as exercising, according to Dr. Tanaka.
I recently wrote a blog discussing metabolic syndrome and therein indicated there is not a direct correlation between obesity and diet. During this conference, Dr. John Hall lectured on the recent advances in CVD and obesity. He suggested that epigenetic transmission of obesity in humans (and others) is associated with increased adiposity and insulin resistance, depletion of nuclear protein, influence chromatin conformation, and altered germ cell methylation and gamete micro RNA.
The new concurrent session Clinical Practice Clinical Science and Primary Care tracks did not go unnoticed. Although I did not get to attend many of these sessions, I did pass them to see that they were well attended. I did attend some of the lunch meetings and they were very insightful. Please refer to my Twitter to see my detailed notes. As mentioned in my pre-conference blog, with all the sessions that were available one should not have had an issue meeting the goals outlined in the program by coordinators (infra vide). Several sessions that met the interest of all researchers/clinicians, early career, and everyone in between. Not a person that attended Hypertension18 could say they could not find a learning opportunity at the Joint Hypertension 2018 Scientific Sessions! Even if one was merely a passerby, there was a session relevant to them. For example, I was on my way to get coffee when I encountered Drs. Yagna Jarajapu from North Dakota State University and Daniel Batlle from University of Chicago discussing research concerning STZ diabetic Foxn1 mice that were ischemic for several days. Subsequently, Eric Metterhausen shared his mission of services (MOS, for you military people) with me as we conversed about field medicine with the United States Public Health Services (USPHS). I did know our US Armed Forces had research officers and divisions of research, but the amount of detail that Major Metterhausen described was a beast that I had not known. Conversations such as these lead to increased mentoring relationship, as well as potential collaborations in research and grant proposals. We all go to conferences to learn, to purchase new research equipment, and to present our data, but we also should not forget to network and build relationships.
Conference Learning Objectives:
- Discuss changes to the AHA/ACC guidelines for the management of hypertension and their clinical implications.
- Describe opportunities to improve blood pressure measurement in the clinical setting to provide more accurate results.
- Identify immune and inflammatory mechanisms that contribute to the development of hypertension and hypertension-related end-organ damage and discuss the research and clinical implications.
- Educate participants about medical approaches for the management of comorbid obesity in patients with hypertension.
- Describe new and emerging strategies for treating resistant hypertension.
- Describe participants on the impact of value-based reimbursement on hypertension management and identify opportunities to improve its management.
See you all in Chicago at Scientific Sessions 2018!!!
- Leave a comment and follow me on Twitter @AnberithaT and @AHAMeetings if you have questions or are interested in something else specifically.

Anberitha Matthews, PhD is a Postdoctoral Fellow at the University of Tennessee Health Science Center in Memphis TN. She is living a dream by researching vascular injury as it pertains to oxidative stress, volunteers with the Mississippi State University Alumni Association, serves as Chapter President and does consulting work with regard to scientific editing.