Deep Dive in HARP Trial
“Coronary Optical Coherence Tomography (OCT) and Cardiac Magnetic Resonance (CMR) Imaging to Determine Underlying Causes of MINOCA in Women” was presented on day 2 of AHA by Dr. Harmony R. Reynolds, MD during the late-breaking trial session. The trial is also simultaneously published in Circulation(1).
MINOCA (Myocardial Infarction with Nonobstructive Coronary Arteries) is quite a contemporary diagnosis. The term was initially coined by Dr. Beltram in an editorial, in response to a Swedish paper that described the cardiac magnetic resonance imaging findings in patients that had presented with myocardial infarction however did not have any significant coronary artery disease on cardiac catheterization(2). MINOCA affects 6-15% of the patients presenting with MI and disproportionately affects women(1). In 2017, The European Society of Cardiology developed the first international position article on MINOCA and proposed the following MINOCA criteria: (a) AMI criteria as defined by the “Third Universal Definition of Myocardial Infarction”; (b) nonobstructive coronary arteries as per angiographic guidelines, with no lesions ≥50% in a major epicardial vessel; and (c) no other clinically overt specific cause that can serve an alternative cause for the acute presentation (3). Fundamental to the definition of MINOCA is the diagnosis of AMI with an elevated cardiac biomarker, typically a cardiac troponin >99th percentile with a rise or fall in the level on serial assessment. Although elevated troponin levels are indicative of myocyte injury with the release of this intracellular protein into the systemic circulation, the process is not disease-specific and can result from either ischemic or nonischemic mechanisms. MINOCA thus, becomes a working diagnosis. The role of CMR is crucial to establish the etiology in these patients. In 2019, an AHA statement paper on MINOCA, presented a stepwise diagnostic approach to evaluate the etiology(4). This paper proposed the use of coronary imaging after the CMR diagnosis of MI was established to further evaluate coronary etiology in absence of significant atherosclerotic disease. Earlier this year, ESC NSTEMI guidelines suggested class IB indication to perform CMR in patients with MINOCA, recommended use of traffic light diagnostic algorithm, and mentioned the use of OCT for the detection of unrecognized causes at coronary angiography, especially in suspected cases of thrombus, plaque rupture or erosion or SCAD(5).
The goal of the Women’s Heart Attack Research Program (HARP) was to implement an imaging protocol to evaluate the underlying causes of MINOCA, in order to guide clinical practice.
They enrolled 301 women presenting with a diagnosis of MI before the coronary angiography was done, in a prospective manner. 170 patients were diagnosed with MINOCA, out of which 145 had OCT imaging while 116 underwent CMR. The study established the cause of MINOCA in 84.5% of the women who underwent multi-modality imaging (98/116), compared with either OCT or CMR alone. OCT was able to identify culprit lesion in 46% of the patient while 74% of the patients had abnormal CMR. 53% of the patients had late gadolinium enhancement or edema in the coronary territory and ischemic pattern while almost 21% of patients were found to have myocarditis, stress-induced cardiomyopathy, or other nonischemic cardiomyopathies. Almost 15.5% of patients had no identifiable mechanism by OCT or CMR. Half of the patients with ischemic patterns on CMR didn’t have any culprit lesion on OCT. Alternative mechanisms of MI like coronary spasm or thromboembolism leading to MI are suggested in those patients. The study however didn’t perform any provocative testing to induce spasm. Similarly, 40% of the patients with normal CMR had culprit lesion on the OCT. This is lower compared to the latest CMR MINOCA studies where a diagnosis was established up to 87% of the cases(6). Whether these findings are due to shorter duration of ischemic injury or due to longer time between diagnosis of MI and CMR or maybe due to overestimation of the prevalence of abnormalities on OCT given the blinded core laboratory review, remains the point of discussion.
The authors conclude that the Multi-modality imaging with coronary OCT and CMR identified potential mechanisms in 84.5% of women with a diagnosis of MINOCA in this observational study. The study was not designed to test the outcomes and further research is needed to establish if the OCT improves outcomes in patients with a working diagnosis of MINOCA. I am not certain if the trial will impact any OCT recommendation class in future guidelines given the absence of the outcome data and observational nature of the trial. The trial also suggested simultaneous use of OCT and CMR in cases of MINOCA however perhaps establishing the diagnosis MI with CMR, excluding myocarditis and nonischemic cardiomyopathy, in cases with a working diagnosis of MINOCA remains the key. As suggested by the diagnostic algorithm in the guidelines, once the MI diagnosis is established, OCT may be used to evaluate coronary mechanisms, however till the outcome data with OCT is available, this will probably depend on the preference of the clinical cardiologist and local availability. Given more than half of the patients with ischemic pattern on CMR had no culprit lesion on OCT in this trial, we may need more data before recommending regular simultaneous use of OCT and CMR.
References:
- Coronary Optical Coherence Tomography and Cardiac Magnetic Resonance Imaging to Determine Underlying Causes of MINOCA in Women | Circulation [Internet]. [cited 2020 Nov 15]. Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.052008
- Beltrame JF. Assessing patients with myocardial infarction and nonobstructed coronary arteries (MINOCA). Journal of Internal Medicine. 2013;273(2):182–5.
- Agewall S, Beltrame JF, Reynolds HR, Niessner A, Rosano G, Caforio ALP, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017 Jan 14;38(3):143–53.
- Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association | Circulation [Internet]. [cited 2020 Nov 15]. Available from: https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000670
- 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation | European Heart Journal | Oxford Academic [Internet]. [cited 2020 Nov 15]. Available from: https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehaa575/5898842
- Troponin-positive chest pain with unobstructed coronary arteries: incremental diagnostic value of cardiovascular magnetic resonance imaging | European Heart Journal – Cardiovascular Imaging | Oxford Academic [Internet]. [cited 2020 Nov 15]. Available from: https://academic.oup.com/ehjcimaging/article/17/10/1146/2197117
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”


 It has been well accepted that atherosclerosis is the result of chronic inflammation. I have spent several years exploring the role endocannabinoids, lipid-based neurotransmitters that bind to receptors that are expressed throughout the peripheral and central nervous system, play in decreasing oxyradical derived inflammation. Under normal conditions, lipids are metabolized and excreted from the body. It is my belief we have an endogenous mechanism that maintains balance within the vascular system that protects our arteries from becoming damaged; however, in the event of an injury the immune system is activated leading to cardiovascular dysfunction.
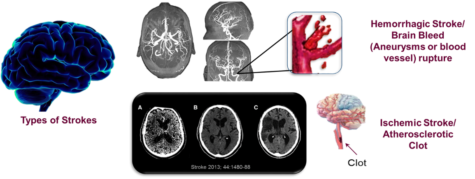
It has been well accepted that atherosclerosis is the result of chronic inflammation. I have spent several years exploring the role endocannabinoids, lipid-based neurotransmitters that bind to receptors that are expressed throughout the peripheral and central nervous system, play in decreasing oxyradical derived inflammation. Under normal conditions, lipids are metabolized and excreted from the body. It is my belief we have an endogenous mechanism that maintains balance within the vascular system that protects our arteries from becoming damaged; however, in the event of an injury the immune system is activated leading to cardiovascular dysfunction.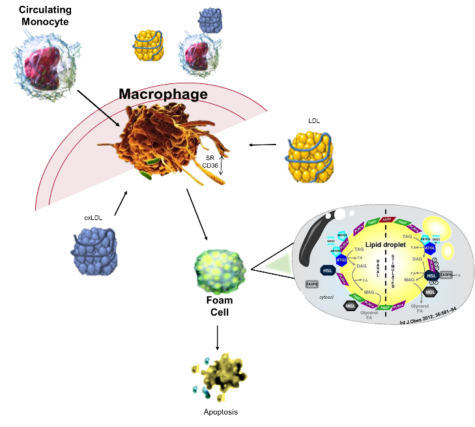 All strokes are not alike, they include ischemic, hemorrhagic, and transient ischemic attacks (TIA). Although older persons are thought to be the primary risk group for strokes, children and fetus can potentially be included in the risk population. The most common type is ischemic stroke caused by clots occluding the blood flow to the brain. The clots can be from congenital heart defects, sickle cell disease, and trauma that injures a large artery; however, they can also be a consequence of high cholesterol, oxLDL, and blood clots as well as
All strokes are not alike, they include ischemic, hemorrhagic, and transient ischemic attacks (TIA). Although older persons are thought to be the primary risk group for strokes, children and fetus can potentially be included in the risk population. The most common type is ischemic stroke caused by clots occluding the blood flow to the brain. The clots can be from congenital heart defects, sickle cell disease, and trauma that injures a large artery; however, they can also be a consequence of high cholesterol, oxLDL, and blood clots as well as