Join the race against the clock: Controlling for age in cardiovascular disease

The race against aging has already started. People who want part of this race see the limitless opportunities humans will have if aging is taken out of the equation. Humans will be able to live longer with their loved ones, go back to University when they are 70 years old to study this long-dreamed profession they always wanted to try or take the time to go through every single item on their bucket list, no matter how long the list is. Others are worried about what awaits them at the finish line of the race and what sacrifices will have to be made along the way. They argue that aging is the core of our existence and the reason why we make the choices we make every day. If humans don’t age, will they still find a reason to live and would this type of life be worth living? Regardless of people’s scattered opinions, the remaining question to be answered in our race against the clock is: Can we age disease-free?
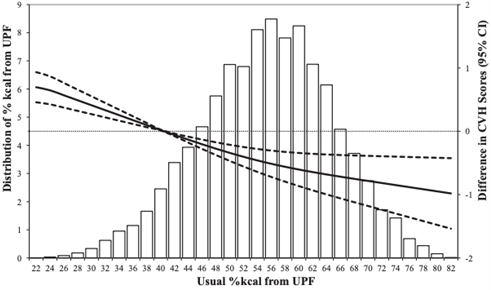
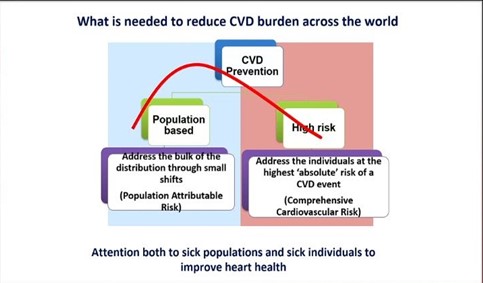
As humans began to live longer dying less of problems such as hunger, wars and infections, they were faced with a new type of problem: chronic diseases. As we age and get exposed to different environmental and lifestyle factors, a set of biological and functional changes in our bodies lead to the development of chronic diseases such as cardiovascular diseases (CVD), diabetes, cancer, dementia, arthritis, and the list goes on. Notorious for being the ‘number 1 killer in the world’, preventing CVD has been one of the top priorities in our fight against aging. Age is the best predictor of CVD death, and despite years of research and large amounts of funding spent on biomarker discovery, there are currently no better predictors of CVD death than the age of a person and these are some of the reasons why.
Large blood vessels tend to become stiffer over time as they accumulate more collagen (due to an increase in TGF-b activity leading to collagen synthesis from smooth muscle cells) and lose their elastin content (because of higher metalloproteases and cathepsin activity). This leads to a chronic increase in systolic blood pressure which is worsened by the rise of catecholamines levels usually seen during aging. Both phenomena contribute to left ventricular dysfunction and hypertrophy due to the increase in myocardial oxygen demand. Calcification is another hallmark of aging that also contributes to vessel stiffness and induces stenosis. As we age, skeletal calcium is released and tends to accumulate in the vascular structures.
Apart from leading to vessel stiffness, aging causes the vascular endothelial cell (EC) barrier to become dysfunctional. ECs play a crucial role in maintaining vessel integrity and homeostasis by balancing vasodilatory and vasoconstricting functions and by aligning the vessels with an anti-thrombotic surface. Disruption of this protective barrier over time is characterized by ECs undergoing oxidative stress, reduced nitric oxide (a potent vasodilator) production, increased expression of adhesion molecules (ICAM and VCAM) and secretion of inflammatory chemokines (CXCL8) and cytokines (IL-1b and IL-6). The initiating event of atherosclerosis development starts with endothelial dysfunction which gives way for monocyte infiltration and subsequent foam cell formation contributing to plaque development.
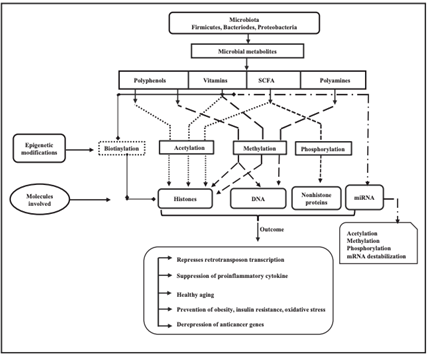
At the molecular level, changes affecting the genome and epigenome are a fundamental feature of aging. With age, the clonal diversity of hematopoietic stem cells decreases resulting in the predominance of one clone. In recent years, clonal hematopoiesis of indeterminate potential (CHIP), which occurs as a result of mutations in transcriptional regulators (DNMT3A, TET2 and ASXL1), was found as a novel CVD risk factor, thereby linking genetic mutations in hematopoietic stem cells, aging and CVD. The number of endothelial progenitor cells also decreases over time which reduces angiogenesis capacity and capillary density leading to microvascular disease (such as peripheral artery disease).
The shortening of chromosome telomers is another molecular change related to aging. As cells replicate, telomeres get shorter until cellular senescence is triggered. Cellular senescence is a cellular protective mechanism that activates NK cells to remove cells with defective genetic material via apoptosis. It has been shown that patients with reduced leukocyte telomere length have increased risk of atherosclerosis. An atherosclerotic plaque, rich in inflammatory cells and trans-differentiated smooth muscle cells, is a dense hypoxic environment characterized by the presence of reactive oxygen species which also induce DNA damage and senescence.
Current therapies for atherosclerosis target some of the pathways of aging highlighted above. While statins are known to reduce plaque lipid content and inflammation, in parallel, they tend to increase calcification leading to vascular stiffness. On the other hand, anti-hypertensive treatments offer benefits beyond reducing CVD mortality, but also decreasing dementia. Recently, novel therapies targeting aging in CVD have focused on stem cell therapy. However, clinical trials using cell therapy to improve left ventricular dysfunction or to reduce cardiovascular events have shown no or modest benefit. This may be because autologous cell therapy of stem cells that already have an ‘aging’ phenotype is not ideal, and these cells may require ex vivo reprograming to improve treatment efficiency.
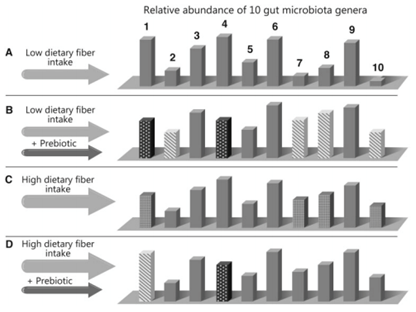
Since many age-related diseases have similar underlying molecular mechanisms driving them, the future for treating chronic diseases will rely on targeting the mechanisms of aging rather than treating the disease itself. Some of the best ways to slow down aging is by being active, controlling blood glucose levels, opting for diets rich in antioxidants and fibers and introducing low calorie intake periods during the day. However, this usually requires a substantial effort and serious lifestyle changes on our behalf. But, since research on anti-aging therapies and senolytic drugs is booming, it might be possible to slow down aging by taking one or two pills a day without ever needing to change the routines that we are so comfortable with.
References
- Paneni F, Diaz Cañestro C, Libby P, Lüscher TF, Camici GG. The Aging Cardiovascular System: Understanding It at the Cellular and Clinical Levels. J Am Coll Cardiol. 2017 Apr 18;69(15):1952–67.
- Quyyumi AA, Vasquez A, Kereiakes DJ, Klapholz M, Schaer GL, Abdel-Latif A, et al. PreSERVE-AMI. Circ Res. 2017 Jan 20;120(2):324–31.
- Brouilette SW, Moore JS, McMahon AD, Thompson JR, Ford I, Shepherd J, et al. Telomere length, risk of coronary heart disease, and statin treatment in the West of Scotland Primary Prevention Study: a nested case-control study. The Lancet. 2007 Jan 13;369(9556):107–14.
- Koopman JJE, Kuipers RS. From arterial ageing to cardiovascular disease. The Lancet. 2017 Apr 29;389(10080):1676–8.
- Jaiswal S, Libby P. Clonal haematopoiesis: connecting ageing and inflammation in cardiovascular disease. Nat Rev Cardiol. 2020 Mar;17(3):137–44.
- Antonangeli F, Zingoni A, Soriani A, Santoni A. Senescent cells: Living or dying is a matter of NK cells. J Leukoc Biol. 2019 Jun;105(6):1275–83.
- What is the Age of My Heart? – Calculate Your Own Heart Age • MyHeart [Internet]. MyHeart. 2015 [cited 2022 May 16]. Available from: https://myheart.net/articles/what-is-the-age-of-my-heart-calculate-your-own-heart-age/
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”