The Protective Role of Anti-Hypertension Medication Among Patients with Comorbidities for COVID-19 Outcomes
Millions of people around the world take Angiotensin-converting enzyme inhibitors (ACEi) and Angiotensin II receptor blockers (ARB) to manage hypertension, heart failure, and coronary artery disease. Concerns of ACEi and ARB potentially increasing the risk of COVID-19 illness severity and mortality among vulnerable populations heightened once scientists reported that risk factors for developing complications included being older, male, and having cardiovascular comorbidities1. One comprehensive study using over 17,000 primary care records found that chronic heart disease has a hazard ratio of 1.57 for COVID-19 related death and the hazard ratio remained high at 1.17 even when accounting for confounding variables, suggesting that people with heart disease are at increased risk of mortality2. In the same study, high blood pressure or hypertension diagnoses were associated with hazard ratio of 0.89, a lower risk of COVID-19 mortality compared to people with normal blood pressure, but insight into how age, sex, comorbidities, and medications influence outcomes were not directly addressed. Such findings fueled a debate about whether ACEI/ARB should be maintained or withdrawn in patients with COVID-19.
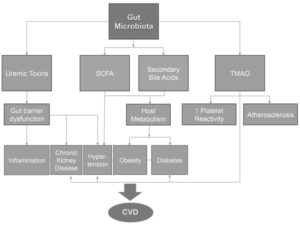
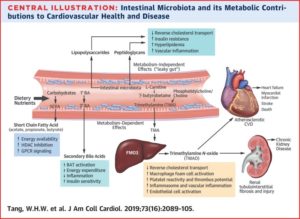
The role of ACEi and ARBS drugs in COVID-19 outcomes among cardiovascular patients also became a point of interest due to their mechanism of action in the human body. ACEi and ARB act on the renin-angiotensin-aldosterone system (RAAS), a hormone system important for regulating blood pressure, fluid balance, and inflammation processes that affect cardiovascular health outcomes. While ACEi and ARB drugs are used as the first line of treatment to manage vasoconstriction, there is a question as to how these medications can alter the RAAS balance. In a previous blog, we discussed how the SARS-CoV-2 virus uses the of angiotensin-converting enzyme 2 (ACE2) receptor to enter host target cells3. This receptor not only acts as the entry point for the virus, but normally acts as a crucial element for regulating RAAS biochemical processes. The inflammatory, tissue damaging, and vasoconstriction effects of Angiotensin II (Ang II) in the body are mitigated by ACE2 activity, and ARB and ACEi drugs also target the Ang II protein4. COVID-19 related research has provided a new understanding of how underlying disease states, behavioral habits like smoking, or genetics could influence ACE2 activity in the body. The unique collaboration between clinicians and scientists during the COVID-19 pandemic has provided new mechanistic insight about how the complex RAAS pathway and the factors that influence disease progression.
Ongoing population studies such as The International Study of Inflammation in COVID-19 (ISIC) and The Michigan Medicine COVID-19 Cohort (M2C2) make use of detailed medical records bio-banked human samples, and advanced statistical modeling to evaluate the potential benefits and harms of ACEi and ARB medications. Using stored blood samples and electronic medical records from patients hospitalized specifically for COVID-19, researchers were able to assess for an association between ACEi or ARB use and in-hospital patient outcomes, such as requiring mechanical ventilation or admission into intensive care. The research team overseeing the ISIC and M2C2 studies analyzed the health outcomes of about 1,600 people hospitalized for COVID-19 and reported that patients taking ACEi or ARB had about 10% mortality compared to 14% who were not on those medications5. Among those taking medications, 24% of patients required ventilation during hospitalization, compared to 20% of those not any treatment. These results were surprising as people taking medication also had significantly more comorbidities such as diabetes compared with the non-ACEi/ARB group. Knowing that people who use ACE inhibitors or ARB are not more susceptible to severe COVID-19 illness or increased risk of mortality during hospitalization has now led to the widely accepted practice of not discontinuing these drugs in people who are infected with SARS-CoV-2. In fact, people on anti-hypertensive medication had lower levels of inflammation biomarkers during hospital admission compared to those who don’t take ACEi and ARB drugs. This insight suggests that ACEi/ARB drugs could counter the inflammatory effects of COVID-19, which could be an interesting future direction of this research. Large scale studies have been valuable for providing evidence on how to mitigate detrimental outcomes during the COVID-19 pandemic and future findings will continue to influence guidelines for monitoring cardiovascular homeostasis, targeting treatments for vulnerable populations, and managing chronic illnesses.
References:
- Patel AB, & Verma A. (2020). COVID-19 and Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: What Is the Evidence? JAMA. https://doi.org/10.1001/jama.2020.4812
- Williamson EJ, Walker AJ, Bhaskaran K, et al. (2020). Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-436. doi:1038/s41586-020-2521-4
- Raizada MK, & Ferreira AJ, (2007). ACE2: A New Target for Cardiovascular Disease Therapeutics. Journal of Cardiovascular Pharmacology, 50(2), 112–119. https://doi.org/10.1097/FJC.0b013e3180986219
- Monterrosa Mena, J. ACE-2 and Immune System Changes in Smokers May Underlie COVID-19 Vulnerability. https://earlycareervoice.professional.heart.org/ace-2-and-immune-system-changes-in-smokers-may-underlie-covid-19-vulnerability/
- Pan N, Hayek S, the ISIC Group, et al. (2021). Angiotensin‐Converting Enzyme Inhibitors, Angiotensin II Receptor Blockers, and Outcomes in Patients Hospitalized for COVID‐ Journal of the American Heart Association, 10(24), e023535. https://doi.org/10.1161/JAHA.121.023535
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”
 Blood pressure is the force that blood applies to the walls of arteries as it’s pumped throughout the body.
Blood pressure is the force that blood applies to the walls of arteries as it’s pumped throughout the body.
 We are faced with a number of changes in our lives. The old saying, “life happens” generally means take the changes as they come and keep it moving. The human body is not equipped to distinguish between distress and eustress. Amazing life changes happens such as getting acknowledged for an accomplishment, passing the preliminary exams for a PhD program, getting the job of your dreams, or even getting the funding you have worked so hard to apply for consideration. Contrarily, changes that can be viewed as less than optimal such as being passed over for a promotion, losing the sole source of your family’s income, death of dreams, and rejection are all sources of stress. Good or bad, these events affect hypertensive rates potentially leading to a more serious chronic illness such as heart attacks, strokes, or even metabolic disease.
We are faced with a number of changes in our lives. The old saying, “life happens” generally means take the changes as they come and keep it moving. The human body is not equipped to distinguish between distress and eustress. Amazing life changes happens such as getting acknowledged for an accomplishment, passing the preliminary exams for a PhD program, getting the job of your dreams, or even getting the funding you have worked so hard to apply for consideration. Contrarily, changes that can be viewed as less than optimal such as being passed over for a promotion, losing the sole source of your family’s income, death of dreams, and rejection are all sources of stress. Good or bad, these events affect hypertensive rates potentially leading to a more serious chronic illness such as heart attacks, strokes, or even metabolic disease.

 Getting to Hawaii was quite the event! I underestimated the flight and how I would feel with such time zone changes. However, the International Stroke Conference 2019 (#ISC19) was worth all the efforts. The meeting objectives were sufficiently described in the program book and
Getting to Hawaii was quite the event! I underestimated the flight and how I would feel with such time zone changes. However, the International Stroke Conference 2019 (#ISC19) was worth all the efforts. The meeting objectives were sufficiently described in the program book and