Lilly’s MounjaroTM (Tirzepatide): A New Sheriff in Town

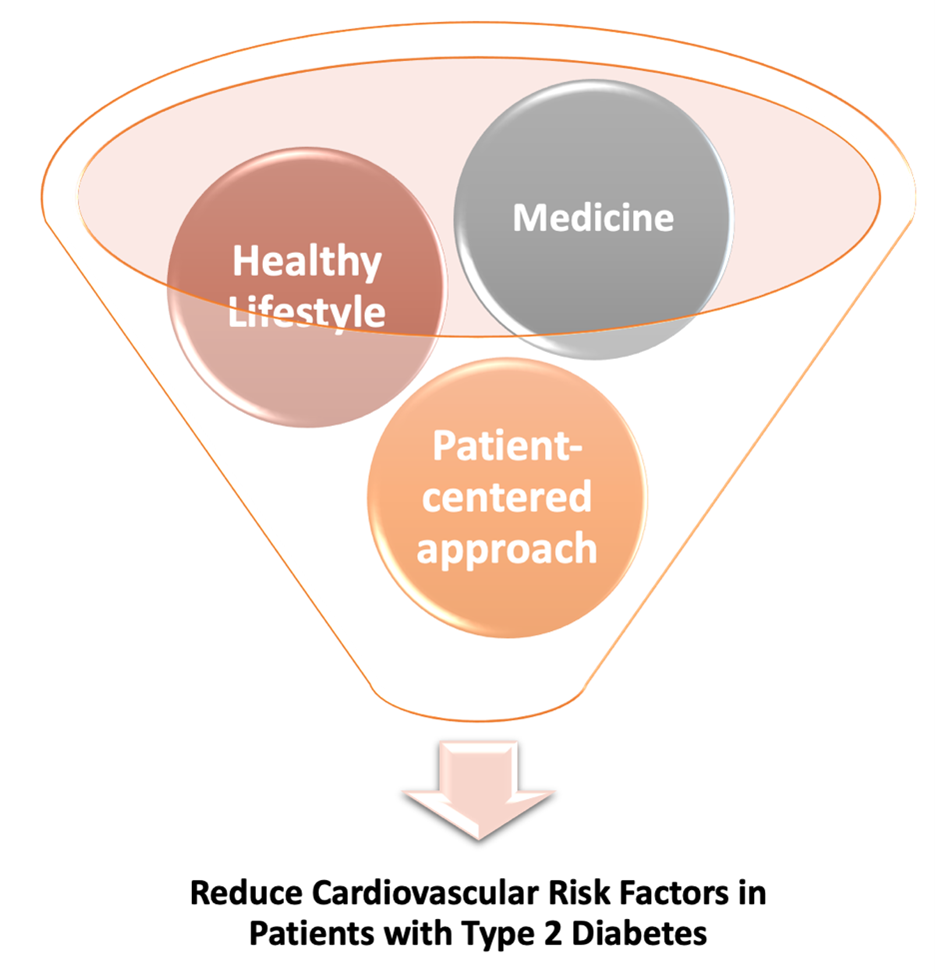
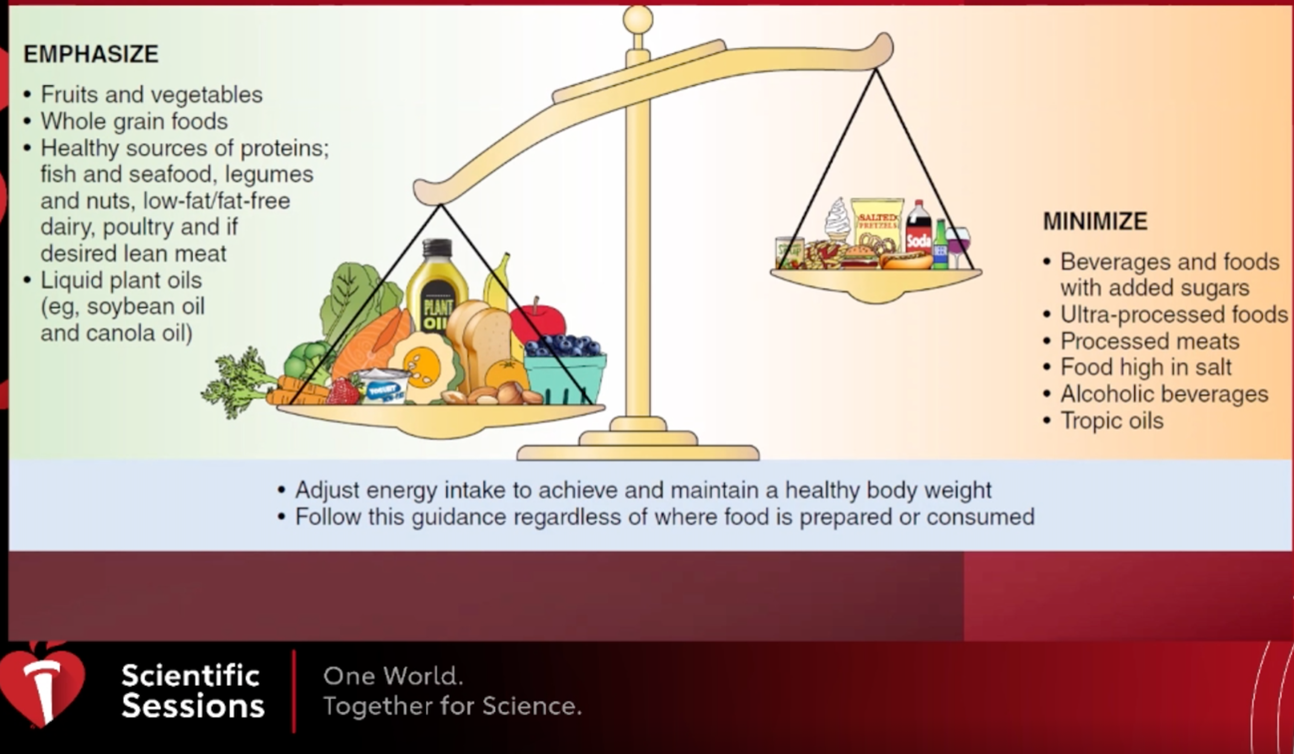
The prevalence of diabetes is increasing at an alarming rate, with more than 34 million Americans suffering from diabetes1. Patients with type 2 diabetes make up 90% to 95% of total diabetes cases1. Type 2 diabetic patients either do not produce enough insulin or develop insulin resistance, resulting in elevation of their blood glucose levels2. The U.S. Food and Drug Administration (FDA) recently, as an adjunct to diet and exercise, approved Eli Lilly and Company’s MounjaroTM (tirzepatide) injection (under the skin, once a week) for Type 2 diabetic patients to control hyperglycemia. Mounjaro will be offered in 6 different doses, 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg, in an auto-injected pen with a pre-attached hidden needle. However, Mounjaro has not been designated to use in Type 1 diabetic patients and is not yet tested for patients with pancreatitis or children under 18 years of age3.
Mechanism of Action of MounjaroTM (tirzepatide):
Eli Lilly and Company’s new drug is a dual agonist of glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor. GIP and GLP-1 are incretin hormones that are released from intestine upon ingestion of food. GLP-1 stimulates the release of insulin from beta cells of pancreas, increases the number and volume of beta cells, and decreases the levels of glucagon, a hormone also released by pancreas that instructs the liver to release stored glucose in the circulation2. Similarly, GIP also fuels insulin release, promotes beta cell production, and prevents destruction of beta cells2. In Type 2 diabetes, patients do not respond properly to incretin hormones. Mounjaro battles this issue by triggering the activation of GIP and GLP-1 receptor2.
Side Effects of MounjaroTM (tirzepatide):
The most common reported side effects, in at least 5% of patients, are nausea, diarrhea, reduced appetite, vomiting, constipation, indigestion, and abdominal pain. Mounjaro may cause severe side effects including hypoglycemia, pancreatitis, allergic reaction, kidney problems, gallbladder problems, and changes in vision. Further, a warning regarding thyroid cancer is issued; therefore, Mounjaro is not advised to use in patients with personal or family history of Medullary Thyroid carcinoma or Multiple Endocrine Neoplasia Syndrome Type 23.
SURPASS clinical trial program of MounjaroTM (tirzepatide):
The SURPASS trials evaluated the efficacy and safety of Mounjaro for Type 2 diabetes as a monotherapy and as an add-on to other standard care medications. Mounjaro was compared as other injectable medicines like semaglutide (GLP-1 mimic), insulin glargine and insulin degludec. Throughout the five global SURPASS studies, Mounjaro exhibited reduction in A1C among participants having Type 2 diabetes from an average of 5 to 13 years3.
- SURPASS-1 (NCT03954834): A 40-week study tested the efficacy and safety of three different doses of Mounjaro (5 mg, 10 mg, and 15 mg) as monotherapy in comparison to placebo in Type 2 diabetic patients (naïve to injectable therapy and utilizing diet and exercise alone). Researchers reported that tirzepatide reduced A1C by 1.8% (with 5 mg) and 1.7% (with 10 mg and 15 mg) as compared to 0.1% with placebo. Further, participants lost weight on an average of 14 lb. (5 mg), 15 lb. (10 mg), and 17 lb. (15 mg) whereas participants in placebo group only lost 2 lb3,4.
- SURPASS-2 (NCT03987919): In this 40-week study, participants were divided in 1:1:1:1 ratio to receive 5 mg, 10 mg, or 15 mg tirzepatide or 1 mg of semaglutide. Mounjaro reduced A1C by 2.0% (5 mg), 2.2% (10 mg) and 2.3% (15 mg) and semaglutide reduced A1C by 1.9%. In a key secondary endpoint, participants in Mounjaro group lost weight by a mean of 17 lb. (5 mg), 21 lb. (10 mg) and 25 lb. (15 mg) in comparison to 13 lb. reduced by semaglutide3,5.
- SURPASS-3 (NCT03882970): A 52-week study compared the efficacy of previous doses of Mounjaro to insulin degludec (insulin analogue) as an add on to metformin with and without SGLT2 inhibitors. The trial reported 1.9% (5 mg), 2.0% (10 mg) and 2.1% (15 mg) reduction in A1C in patients receiving tirzepatide as compared to 1.3% reduction in patients receiving insulin degludec. Interestingly, participants on Mounjaro lost 15 lb. to 25 lb. depending on the dose, but participants taking insulin degludec gained an average of 4 lb3,6.
- SURPASS-4 (NCT03730662): A 104-week study compared the efficacy of Mounjaro (5 mg, 10 mg, 15 mg) to insulin glargine in Type 2 diabetic patients with increased risk of cardiovascular disease. Researchers observed a 2.1% (5 mg), 2.3% (10 mg) and 2.4% (15 mg) reduction in A1C in patients receiving tirzepatide as compared to 1.4% reduction in patients receiving insulin glargine. Participants on Mounjaro lost weight (14 lb. with 5 mg, 20 lb. with 10 mg, and 23 lb with 15 mg), whereas insulin glargine group gained 4 lb3,7.
- SURPASS-5 (NCT04039503): In this 40-week study, the efficacy and safety of Mounjaro as an add on drug to insulin glargine was compared to placebo. An average of 2.1% (5 mg), 2.4% (10 mg) and 2.3%* (15 mg) reduction was observed in Mounjaro group as compared to 0.9% in placebo group. Further, Mounjaro, as an add on drug, reduced body weight by 12 lb. to 19 lb. as compared to placebo group, where participants experienced 4 lb. weight gain3,8.
REFERENCE
- National Diabetes Statistics Report. Accessed January 14, 2022. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- FDA approves trizepatide: A potent new drug for type 2 diabetes. Accessed May 20, 2022. https://www.medicalnewstoday.com/articles/fda-approves-tirzepatide-a-potent-new-drug-for-type-2-diabetes
- FDA arrpvoves Lilly’s MounjaroTM (tirzepatide) injection, the first and only GIP and GLP-1 receptor agonist for the treatment of adults with type 2 diabetes. Accessed May 20, 2022. http://lilly.mediaroom.com/2022-05-13-FDA-approves-Lillys-Mounjaro-TM-tirzepatide-injection,-the-first-and-only-GIP-and-GLP-1-receptor-agonist-for-the-treatment-of-adults-with-type-2-diabetes
- Rosenstock J, Wysham C, Frías JP, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 07 10 2021;398(10295):143-155. doi:10.1016/S0140-6736(21)01324-6
- Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. N Engl J Med. 08 05 2021;385(6):503-515. doi:10.1056/NEJMoa2107519
- Ludvik B, Giorgino F, Jódar E, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 08 14 2021;398(10300):583-598. doi:10.1016/S0140-6736(21)01443-4
- Del Prato S, Kahn SE, Pavo I, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. 11 13 2021;398(10313):1811-1824. doi:10.1016/S0140-6736(21)02188-7
- Dahl D, Onishi Y, Norwood P, et al. Effect of Subcutaneous Tirzepatide vs Placebo Added to Titrated Insulin Glargine on Glycemic Control in Patients With Type 2 Diabetes: The SURPASS-5 Randomized Clinical Trial. JAMA. 02 08 2022;327(6):534-545. doi:10.1001/jama.2022.0078
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”