Late-Breaking Highlights: “To Screen Or Not To Screen And Then What? Studies of Detection and Treatment of AF”
This was an exciting session at AHA 2020 which focused on clinical trials of screening, monitoring, and early intervention in Atrial Fibrillation (AF). Screening of AF is a controversial topic and for individuals >65 years, current AHA guidelines give a Grade 2a recommendation for screening whereas USPSTF guidelines suggest that there is insufficient evidence for screening. In this article, I will be discussing studies that addressed AF screening and their implications on clinical practice with Dr. Stavros Stavrakis who is an electrophysiologist and Associate Professor at the University of Oklahoma Health Sciences Center, Oklahoma City.
Question: What are the important goals when we think about screening for AF?
Dr. Stavrakis: The important goals for screening in AF are to establish a diagnosis of new AF in patients at high risk of stroke so they can be anticoagulated, ultimately reducing the risk of stroke.
There were 3 important trials that addressed AF screening in different patient populations.
SEARCH AF
- In patients who have undergone cardiac surgery and have a higher risk of stroke but no history of pre-operative or pre-discharge AF, what is the risk of developing AF/Aflutter in the sub-acute post discharge period?
- 336 post-cardiac surgery patients (median CHADS2Vasc Score 4) but with little or no AF in the post-operative period (<24 hours of AF but no intent to anticoagulate at discharge) were randomized to continuous cardiac rhythm monitoring vs usual care during the sub-acute post discharge period.
- In the enhanced cardiac rhythm monitoring group 19.6% participants developed AF/Aflutter as compared with 1.7% in the usual care group with an absolute rate difference 17.9% (p<0.001, NNS=6).
Question: What are the implications of this trial on clinical practice?
Dr. Stavrakis: Risk of POAF, although peaking at 48-72hours post-op, is not confined to the index hospitalization, continuous monitoring for POAF can identify AF in a significant proportion of patients (20%) that may need treatment with anticoagulation. Whether anticoagulation improves outcomes in these patients, remains to be determined.
VITAL-AF Trial
- Among older adults (age>65) presenting to primary care visits, does point of care rhythm assessment with a single lead ECG result in increased diagnosis of AF?
- 30,722 patients were randomized to screening vs control.
- Screening did not significantly affect AF diagnosis in the overall study sample (1.74% vs 1.60%, p=0.33)
- Increased likelihood of AF diagnosis at primary care encounter (p<0.02)
- Effectiveness of screening varied by age with effective screening in age>85 (risk difference 1.88%, NNS=53)
- Overall no difference in the initiation of anticoagulation
Question: What are the implications of this trial on clinical practice?
Dr. Stavrakis: There are 2 important implications from this trial.
- Screening everyone age>65 for AF at a single time point is not an efficient way to detect AF, especially if the usual care is very good in detecting AF by pulse palpation or BP device.Screening at age>85 may be more effective than usual care to identify silent AF, but it is uncertain if it changes management or outcomes
mSTOPS
- Can screening for AF by wearing an ECG patch improve clinical outcomes at 3-years?
- 1718 actively monitored participants vs 3371 matched observational controls with analysis of 3-year clinical outcomes.
- Mean duration of follow-up was 29 months
- 11.4% of actively monitored patients developed AF vs 7.3% of matched controls
- No difference in anticoagulation prescription between both arms (45.2% vs 44%, p=0.84)
- 3-year Primary combined end point (death, stroke, systemic embolism or MI) for entire cohort was 4.5 vs 5.5 per 100 person-year (HR 0.79, p<0.01) and for diagnosed AF patients it was 8.4 vs 13.8 per 100 person-year (HR 0.53, p<0.01).
Question: What are the implications of this trial on clinical practice?
Dr. Stavrakis: Clinical outcomes can be improved with AF screening provided these patients are followed up for extended periods of time. However, this was not a randomized trial and unknown confounders may have influenced the outcome.
Question: What are 3 important unanswered questions pertinent to screening of AF?
- What is the impact of AF screening on clinical outcomes? Large studies, adequately powered to detect clinical outcomes, are underway (SAFER, HEARTLINE, GUARD-AF).
- What is the optimal screening intensity that identifies AF which would benefit from anticoagulation?
- What is the minimum AF burden that, if identified with screening, would benefit from anticoagulation?
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”

 At my first two AHA Scientific Sessions, I sat in the Main Event Hall, shoulder-to-shoulder with my co-fellows, eagerly awaiting the results of the Late Breaking Clinical Trials and guideline updates. I remember whispers cascading across the room after the presentation of NEAT-HFpEF in 2015 and the hundreds of cellphones in the air snapping pictures of the hypertension guideline release in 2017. This year as an AHA Early Career Blogger, I learned the results of the Late Breaking Clinical Trials with other news writers at embargoed media briefings. These intimate press conferences are routinely offered to health care journalists at major medical meetings and by top medical journals. Members of the media receive early access to manuscripts and data and discuss trial findings with investigators and outside experts with the understanding that nothing should be published until after trial results are publicly released. Generally, media pieces are published very soon after the embargo is lifted. At my first embargoed briefing, I heard one reporter’s question that has spurred me to imagine a new, more inclusive future for scientific meetings.
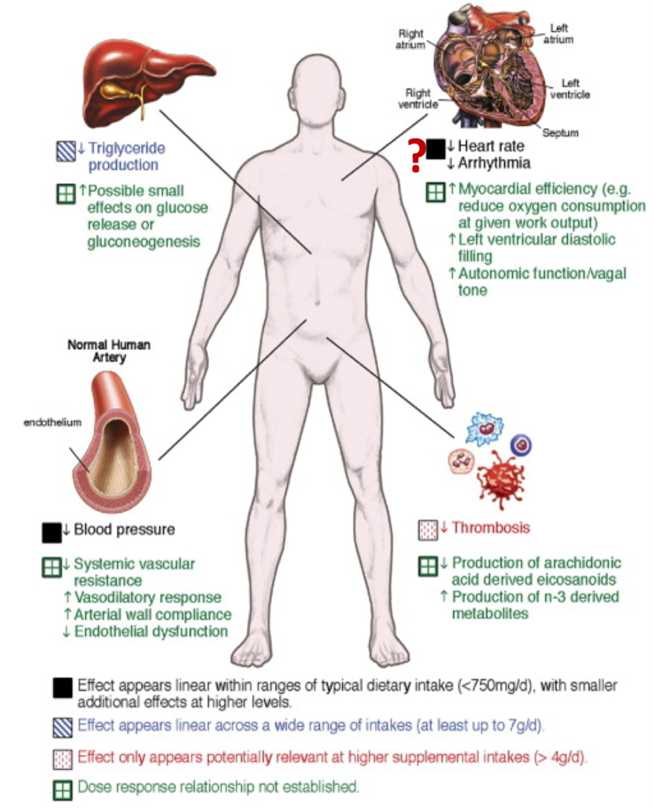
At my first two AHA Scientific Sessions, I sat in the Main Event Hall, shoulder-to-shoulder with my co-fellows, eagerly awaiting the results of the Late Breaking Clinical Trials and guideline updates. I remember whispers cascading across the room after the presentation of NEAT-HFpEF in 2015 and the hundreds of cellphones in the air snapping pictures of the hypertension guideline release in 2017. This year as an AHA Early Career Blogger, I learned the results of the Late Breaking Clinical Trials with other news writers at embargoed media briefings. These intimate press conferences are routinely offered to health care journalists at major medical meetings and by top medical journals. Members of the media receive early access to manuscripts and data and discuss trial findings with investigators and outside experts with the understanding that nothing should be published until after trial results are publicly released. Generally, media pieces are published very soon after the embargo is lifted. At my first embargoed briefing, I heard one reporter’s question that has spurred me to imagine a new, more inclusive future for scientific meetings. On Sunday of Sessions, I joined other health care reporters for the VITAL and REDUCE-IT presentations. In VITAL, 1 gram/day of omega-3 fatty acid supplementation (containing 460 mg of eicosapentaenoic acid [EPA] and 380 mg of docosahexaenoic acid [DHA]) was not effective for primary prevention of cardiovascular events in healthy middle-aged adults. In REDUCE-IT, icosapent ethyl (a purified EPA) at a dose of 2 grams twice daily reduced cardiovascular events among patients at risk for or with known cardiovascular disease and with high triglycerides already on statin therapy with good LDL-C control. After both trials were presented, one news writer probed the primary investigators’ thoughts on communicating these results to patients. The reporter wondered if the trials could be interpreted as sending mixed messages about the cardiovascular benefits of omega-3 fatty acids to the general public. Both trials’ primary investigators acknowledged this concern and systematically reviewed the differences in drug composition, patient populations, and study goals that, in their estimation, led to the outcomes. Multiple panelists implored the journalists to integrate these differences into their stories with hopes that consumers and potential patients would be able to understand the distinctions on their own.
On Sunday of Sessions, I joined other health care reporters for the VITAL and REDUCE-IT presentations. In VITAL, 1 gram/day of omega-3 fatty acid supplementation (containing 460 mg of eicosapentaenoic acid [EPA] and 380 mg of docosahexaenoic acid [DHA]) was not effective for primary prevention of cardiovascular events in healthy middle-aged adults. In REDUCE-IT, icosapent ethyl (a purified EPA) at a dose of 2 grams twice daily reduced cardiovascular events among patients at risk for or with known cardiovascular disease and with high triglycerides already on statin therapy with good LDL-C control. After both trials were presented, one news writer probed the primary investigators’ thoughts on communicating these results to patients. The reporter wondered if the trials could be interpreted as sending mixed messages about the cardiovascular benefits of omega-3 fatty acids to the general public. Both trials’ primary investigators acknowledged this concern and systematically reviewed the differences in drug composition, patient populations, and study goals that, in their estimation, led to the outcomes. Multiple panelists implored the journalists to integrate these differences into their stories with hopes that consumers and potential patients would be able to understand the distinctions on their own. After the briefing, I walked to the Main Event Hall to re-experience the Late Breaking Clinical Trials and thought about how we translate these breakthroughs, frequently announced at scientific meetings, to the public and our patients. Recent data suggest that the use of social media at cardiovascular conferences, a key approach to broadcasting late-breaking scientific developments, is rapidly growing. At these meetings, physicians comprise the largest group of Tweeters and compose nearly half of all tweets.1 Identifying the full scope of our social media audience, though, is more elusive. Ensuring veracity in scientific communication has become progressively challenging as the attitudes and tools to perpetuate misinformation have spread. We know that across multiple information domains, false news spreads faster, farther, and deeper than the truth.2 Just this week, Dictionary.com chose “misinformation” as the 2018 word of the year.3 Clinicians and scientists are now especially vulnerable to this insidious erosion of public trust.
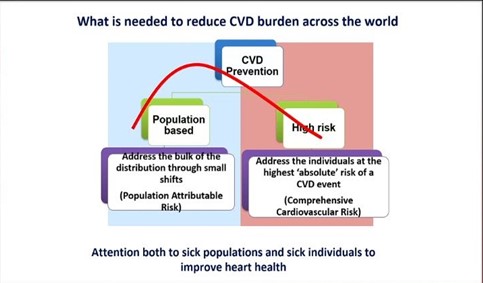
After the briefing, I walked to the Main Event Hall to re-experience the Late Breaking Clinical Trials and thought about how we translate these breakthroughs, frequently announced at scientific meetings, to the public and our patients. Recent data suggest that the use of social media at cardiovascular conferences, a key approach to broadcasting late-breaking scientific developments, is rapidly growing. At these meetings, physicians comprise the largest group of Tweeters and compose nearly half of all tweets.1 Identifying the full scope of our social media audience, though, is more elusive. Ensuring veracity in scientific communication has become progressively challenging as the attitudes and tools to perpetuate misinformation have spread. We know that across multiple information domains, false news spreads faster, farther, and deeper than the truth.2 Just this week, Dictionary.com chose “misinformation” as the 2018 word of the year.3 Clinicians and scientists are now especially vulnerable to this insidious erosion of public trust. How do we combat the propagation of falsehood while encouraging this new democratization of science? I have thought about how the importance of trust was so admirably exemplified in a recent study of blood pressure reduction in black barbershops.4 What if we could leverage our meetings to spread science to where our patients are and with trusted people delivering the message? The AHA has recognized this opportunity and does have programs in place, like “Students at Sessions”, to share Scientific Sessions with non-medical communities.5 Can we imagine a future state of Scientific Sessions where internationally recognized clinicians and scientists deliver a talk at a barbershop or civic center in the host city, where community leaders are invited to participate in panels and plenaries, where large scale cardiovascular risk screenings happen just outside our conference center doors?
How do we combat the propagation of falsehood while encouraging this new democratization of science? I have thought about how the importance of trust was so admirably exemplified in a recent study of blood pressure reduction in black barbershops.4 What if we could leverage our meetings to spread science to where our patients are and with trusted people delivering the message? The AHA has recognized this opportunity and does have programs in place, like “Students at Sessions”, to share Scientific Sessions with non-medical communities.5 Can we imagine a future state of Scientific Sessions where internationally recognized clinicians and scientists deliver a talk at a barbershop or civic center in the host city, where community leaders are invited to participate in panels and plenaries, where large scale cardiovascular risk screenings happen just outside our conference center doors?