Atrial Structure and Function – Methodology of Atrial Strain
“If echocardiographers are to stand still, depend on standard 2D echo imaging using equipment produced a decade ago and not upgraded since, perform “ejectionfractionograms,” focus primarily on the left ventricle and simply ‘‘eyeball’’ the other chambers, and avoid new methods such as strain imaging and contrast echo because they are perceived as ‘‘a waste of time’’, then I fear that echocardiography will be passed by. As the dinosaurs illustrated, we need to adapt and continue to evolve, or face the consequences.” –Alan Pearlman- JASE editor, 2010
My research experience focused on heart failure and atrial function. I conducted medical research on the derivation and validation of novel echocardiographic approaches to myocardial and atrial deformations. I have been heavily involved with all projects using strain echocardiography at Duke University (approximately 50 projects over the last 7 years). I have completed over 10,000 speckle tracking strain measurements analysis on different cardiac diseases and on different cardiac chambers.
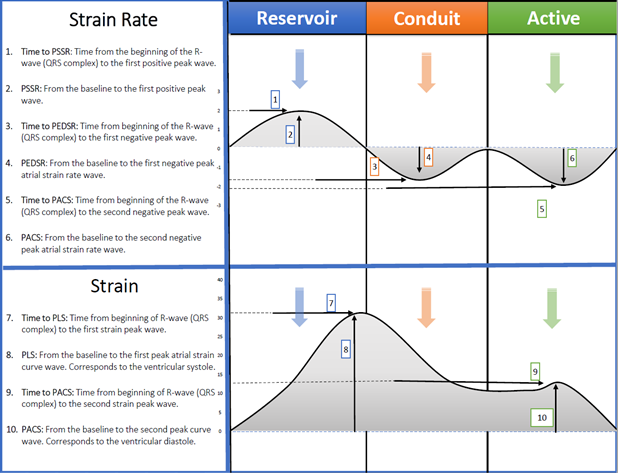
Both left and right atrium function moderate ventricular function through three components:
- Atrial diastole (Reservoir phase) or expansion during ventricular systole. This function is dependent on ventricle longitudinal function, atrial wall elastance and venous return. Reservoir function may increase during physical activity in a normal healthy heart. Increase of this phase help to increase ventricular filling.
- Passive atrial systolic phase (Conduit function) during ventricle early diastole. This phase is dependent on the ventricle end-diastolic pressure. Conduit function does not affect by physical activity.
- Active atrial systolic phase (Active contraction) (when sinus rhythm is present) during ventricle late diastole. This phase is dependent on atrial wall contractile properties and ventricular end diastolic pressure. Active contraction function is affected by physical activity in a normal heart.
Traditionally atrial function was measured indirectly by using volumes. However, this is still not resembling the actual atrial deformation and mechanics. With a high feasibility and reproducibility of speckle tracking strain echocardiography, atrial function is ready to be a part of an echo report in a daily clinical practice.
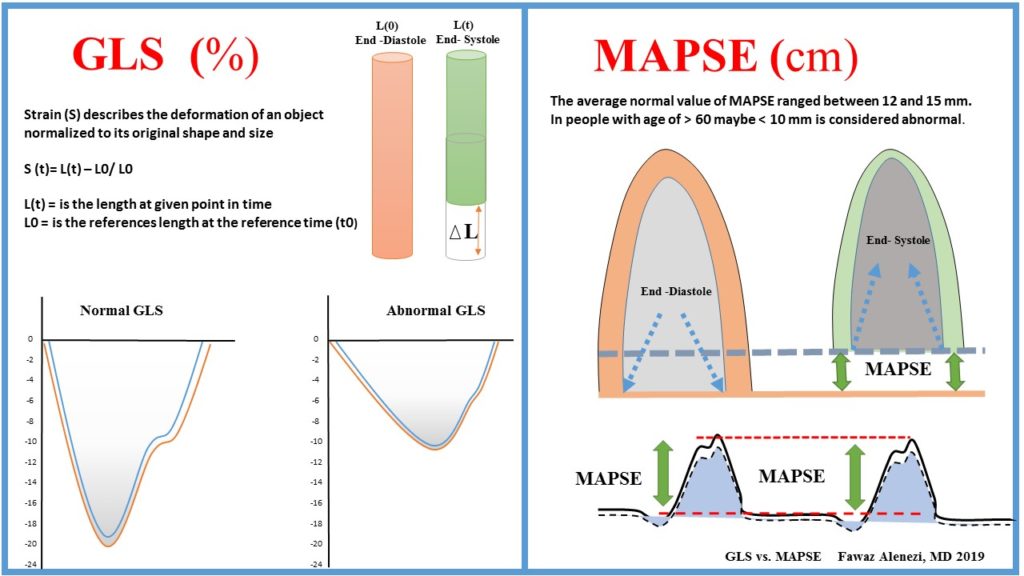
Speckle tracking strain imaging has been around for quite a while and we celebrated the first decade 3 years ago, whereas the technique described in 2004 (Leitman M-JASE) and clinical applications appeared around 2005 (Notomi Y- JACC). Since then, the interest has risen dramatically and so far, we have > 5000 publications on this topic. Left ventricular (LV) ejection fraction (LVEF), the most widely used measure of cardiac function, has important limitations including low sensitivity for incident HF, technique-related variability and does not directly assess LV contractility. Global longitudinal strain (GLS) is the most studied among strain parameters and its prognostic value has been demonstrated in several clinical scenarios.
GLS inter-Vendor variety has dramatically dropped over a short period of time. However, still if we look at the same images with different software vendors, we may have different values. This difference is due to several factors: 1) Image quality and acquisition; 2) Software used; 3) Where to measure (endocardial, myocardial, median); 4) Post-processing of data; 5) Patients age, gender variabilities and loading conditions. With regard to regional (segmental) function, we now have, for the first time, the possibility to measure regional myocardial function. However, I think this is more challenging than GLS, and there is still progress to be made. The challenges become because we have only one segment to work with, and less data to average. Tracking quality becomes more important, regional artifacts matters more, definition of sample position more relevant, and more importantly, we cannot simply measure peak values anymore. For regional analysis, the strain curve shape (not peak values, because peak values can be the same), become critical.
Technical factors that may influence atrial strain values:
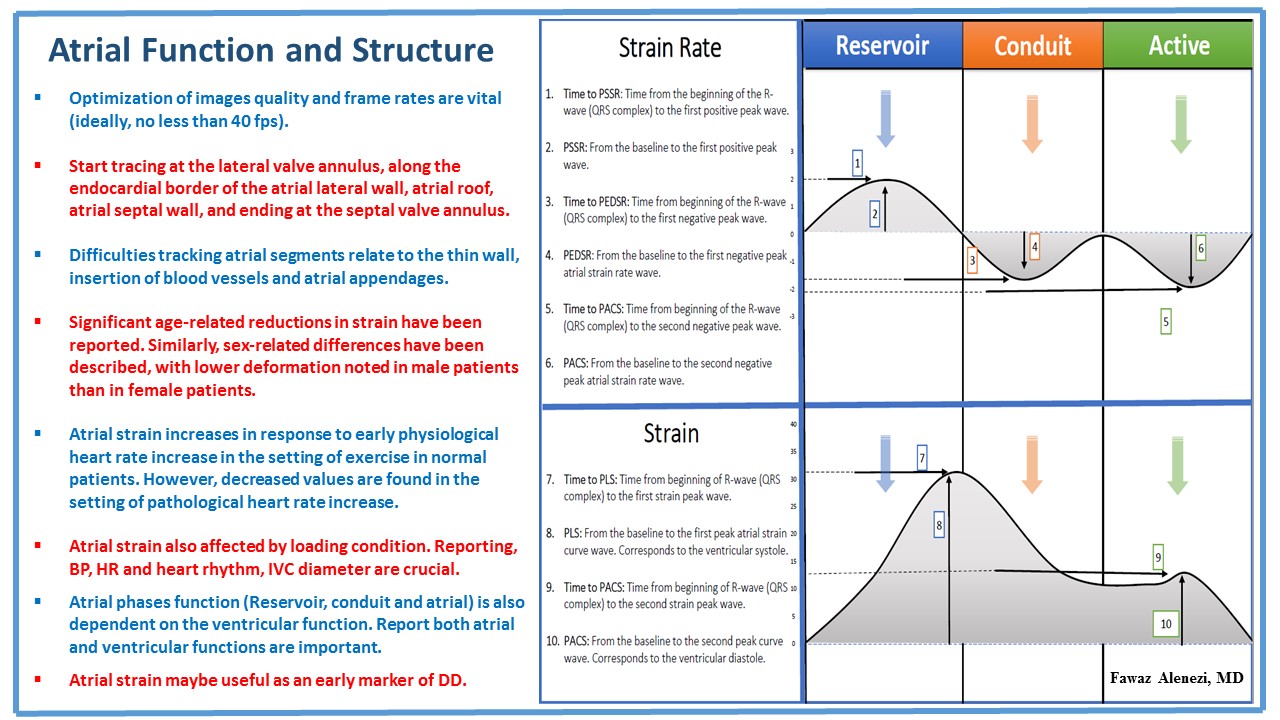
- Optimization of images quality and frame rates are vital (ideally, no less than 40 fps).
- Start tracing at the lateral valve annulus, along the endocardial border of the atrial lateral wall, atrial roof, atrial septal wall, and ending at the septal valve annulus.
- Difficulties tracking atrial segments relate to the thin wall, insertion of blood vessels and atrial appendages.
- Significant age-related reductions in strain have been reported. Similarly, sex-related differences have been described, with lower deformation noted in male patients than in female patients.
- Atrial strain increases in response to early physiological heart rate increase in the setting of exercise in normal patients. However, decreased values are found in the setting of pathological heart rate increase.
- Atrial strain also affected by loading condition. Reporting, BP, HR and heart rhythm, IVC diameter are crucial.
- Atrial phases function (Reservoir, conduit and atrial) is also dependent on the ventricular function. Report both atrial and ventricular functions are important.
- Atrial strain maybe useful as an early marker of DD.
In summary, I think GLS is ready for clinical practice. Its robust, reproducible and has been shown to add unique data that can guide diagnosis and management. I recommend GLS as a valuable complement to traditional function parameters. Further studies are needed to standardize vendors, recognizing specific strain patterns and to determine if there are age, gender variabilities or loading conditions difference.
References:
Myocardial Strain Measured by Speckle-Tracking Echocardiography: Patrick Collier, MD, PHD, Dermot Phelan, MD, PHD, Allan Klein, MD VOL. 69, NO. 8, 2017 – ISSN 0735-1097