Sometimes Less is More
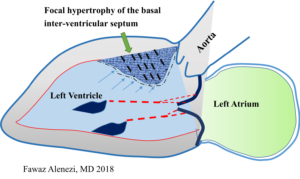
A 64-year-old male presented to emergency room (ER), with complaints of shortness of breath for one day. He had a past medical history of hypertension, end stage renal disease on hemodialysis (HD), and grade I obesity. He reported that he missed his last HD session, which was two days prior to presentation. He denied any chest pain, palpitations, cough, or fever. Patient further mentioned that he was able to walk >10 blocks without any chest pain or shortness of breath until a couple days ago. In the ER, examining physician documented presence of a systolic ejection murmur heard best at the second right intercostal space and bilateral rales, 1+ pedal edema; jugular venous distention of 4cm. Urgent transthoracic echocardiogram (TTE) was ordered by ER physician to further investigate the aortic stenosis (AS) murmur. TTE showed aortic valve area 0.98cm2, mean gradient 32mmHg, aortic jet velocity 3.5m/s; mild left ventricle (LV) concentric hypertrophy with grade 1 diastolic dysfunction, and LV ejection fraction of 60-65%. Subsequently, patient was admitted to cardiac telemetry and primary team consulted renal and cardiothoracic (CT) team for HD and for aortic valve replacement (AVR), respectively.
CT surgery team requested cardiology consult as a part of pre-operative assessment for possible surgical AVR. Physical examination by the attending cardiologist was remarkable for II/VI mid-systolic peaking crescendo-decrescendo murmur with normal carotid pulse upstrokes. Cardiac catheterization was recommended for further evaluation as there was discrepancy between the findings on noninvasive testing and physical examination regarding severity of the AS. Cardiac catheterization revealed non obstructive coronary artery disease (30% stenosis of mid RCA) and moderate AS (aortic valve area 1.38cm2, mean gradient 28mmHg, aortic jet velocity 3.3m/s). During recovery period patient developed hematoma at access site (right groin), which was managed conservatively but resulted in prolongation of his hospital stay by 48 hours. In the meantime, the patient underwent hemodialysis and had symptomatic relief in his dyspnea. He was discharged home to follow up with his outpatient hemodialysis center.
Perspective:
This gentleman presented to ER with complain of shortness of breath after missing a HD session. Although, not incorrect, the systolic murmur heard by ED physician led to a cascade of downstream testing. In fact, the ‘benign’ ‘non-invasive’ testing ordered as a part of comprehensive work-up led to a delay for patient getting the HD session. Physical examination is an essential part of accurate assessment of a patient’s disease process. However, our daily practice has been increasingly occupied by ‘tunneled vision’ of things.
Aortic stenosis (AS) is one of the most common valvular diseases associated with systolic murmur in the elderly population1. An essential part of physical exam of AS is assessing the severity. Munt et al, found significant correlation of physical exam findings like grade of murmur and timing of murmur peak with severity of AS2. Further, delay in carotid upstroke and decreased amplitude was well associated with increasing grade of AS severity as measured by aortic valve area (AVA). Although, one may argue that physical exam is limited by observer expertise and inter-observed variability3, echocardiographic parameters have their own pitfalls. The AVA measurement depends on accurate evaluation of LVOT diameter, which has a variability rate of 5-8% thus providing a significant potential for error4. Further, co-existing LV dysfunction or valvular jets (e.g. MR, AR) can interfere with precise interpretation of echocardiographic parameters.
In summary, the patient should have received urgent HD on presentation. The work up for systolic murmur would have been more appropriate on an outpatient basis. This particular scenario also brings into picture the rising health care costs in the United States, contributed by both additional testing and prolonged hospitalizations. Overall, it is worth concluding that careful physical examination and assessment of the patient is foremost to efficient and ‘do not harm’ philosophy of medicine.
References:
1) Osnabrugge R, Mylotte D, Head SJ, Van Mieghem NM, et al. Aortic Stenosis in the Elderly Disease Prevalence and Number of Candidates for Transcatheter Aortic Valve Replacement: A Meta-Analysis and Modeling Study. J Am Coll Cardiol. 2013;62(11):1002-1012.
2) Munt B, Legget ME, Kraft CD, Miyake-Hull CY, et al. Physical examination in valvular aortic stenosis: Correlation with stenosis severity and prediction of clinical outcome. Am Heart J 1999;137:298-306.
3) Stout KK, Otto CM. Quantification of Valvular Aortic Stenosis. ACC current journal review Mar/Apr 2003.
4) Baumgartner H, Hung J, Bermejo J, Chambers JB, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice.