The controversy over alcohol consumption: Is it good or bad for your heart?
If you go to a party or a professional event, you won’t be surprised to find that alcoholic beverages are served. In fact, in most cases, it’s even expected. Alcohol consumption has been present throughout human history. So do its effects. Excessive drinking has been linked to many health risks, including high blood pressure, heart diseases, stroke, liver diseases, and digestive problems. However, the health effects of light-to-moderate drinking are still in dispute (1). Early evidence showed that light-to-moderate drinking is associated with beneficial effects such as reductions in coronary artery diseases and even in total mortality. This view has been challenged by a few recently published epidemiological studies, which show no direct relationship between the beneficial effects on the heart and light-to-moderate drinking (2).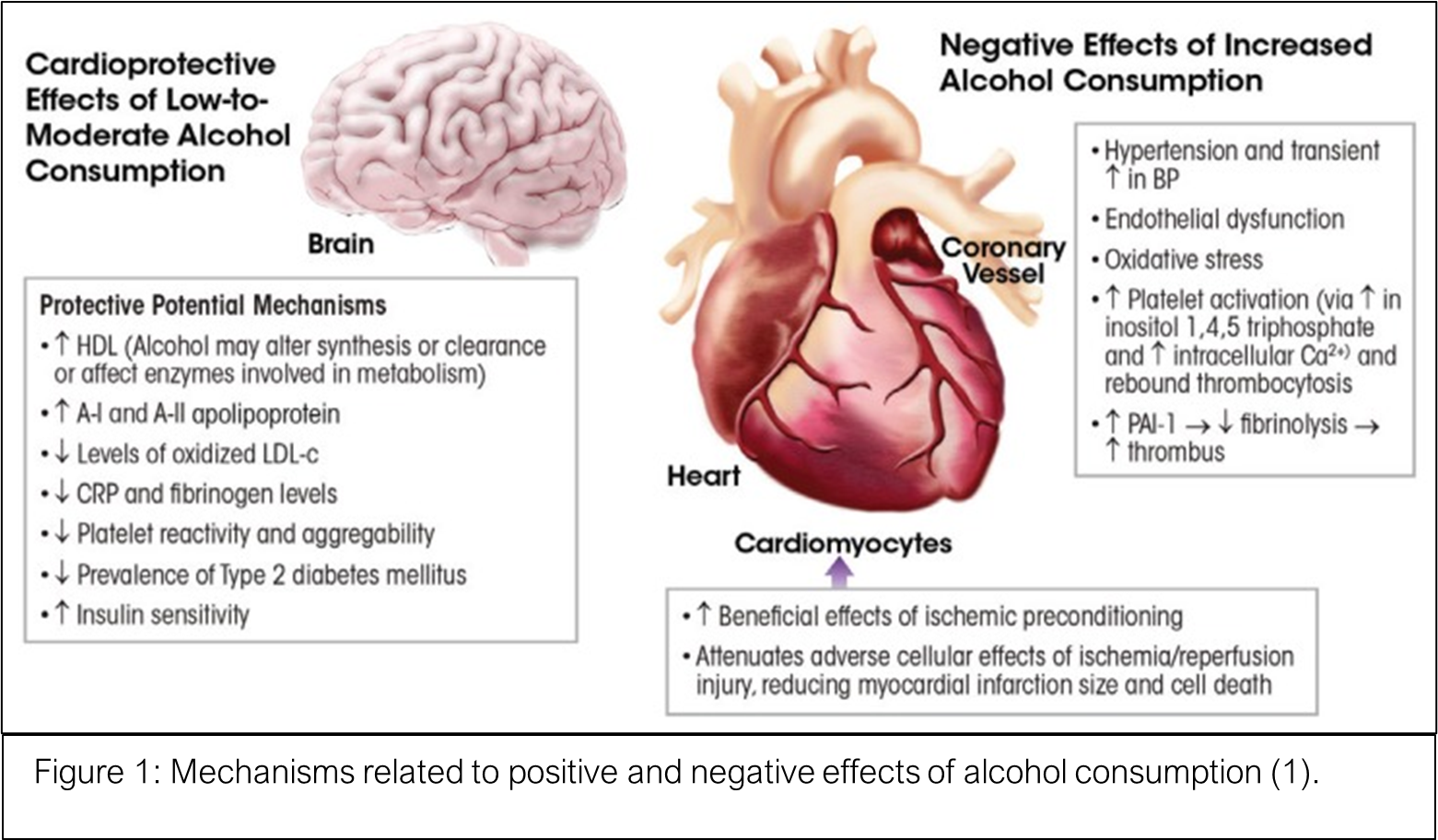
What is light/moderate drinking?
According to National Institute on Alcohol Abuse & Alcoholism, moderate drinking is up to four alcoholic drinks for men and three for women in any single day and a maximum of 14 drinks for men and 7 drinks for women per week. Below that range would be considered light drinking.
Why is there a discrepancy in health risks reports on alcohol consumption?
The obvious:
Confounding factors such as social-economic status, age, genetics, ethnicities, behavior and types of alcoholic beverages play big roles in influencing health effects. It’s not hard to imagine that a wealthy family has more medical resources and more options of choosing a healthy lifestyle, which has lower risks of cardiovascular diseases compared to a low social-economic status family that even consumes the same amount of alcohol. The alcohol metabolism rate differs in different age groups and different populations. The certain population lacks an enzyme, alcohol dehydrogenase, which metabolizes alcohol, that has adverse health effects when drinking alcohol. These confounding factors are important when conducting an epidemiology study. Not all alcoholic drinks are created equal. Bioactive phytochemicals, for example, polyphenols have beneficial effects which can be found in wines. Cocktails usually contain a large amount of sugar, and high sugar consumption are linked to many cardiovascular disorders. It’s hard to tease out the causal effects of light-to-moderate alcohol consumption and the health effects. Moreover, most of the reported works of literature are observational, which leads to more complications when trying to interpret the data.
The less obvious:
Epidemiological study design has evolved rapidly in recent decades. Early studies were focused on interpreting results from limited resources. The lack of enough participants and missing specific details make it impossible to make a causal connection between alcohol consumption and health risks. In 2007, researchers started to encourage epidemiological studies to use large, prospective, and randomized trials when trying to understand the health effects of drinking (3). A recent review just published in Circulation: Heart failure questioned the relationship between alcohol intake and cardiomyopathy and heart failure (4). After analyzing current evidence, they suggest that there is no consensus on the absolute amount alcohol intake which causes cardiomyopathy and heart failure. Another group showed that low alcohol intake has no health benefits, and moderate alcohol intake is associated with adverse effects in heart (5).
To drink or not to drink. There is no one-size-fits-all solution. The jury is still out when it comes to the health effects of light-to-moderate drinking. Monitor your health and consult with your doctor regularly. If it’s not good for you, your body will tell.
REFERENCE
- Piano, M. R. (2017). Alcohol’s Effects on the Cardiovascular System.Alcohol Research : Current Reviews, 38(2), 219–241.
- Biddinger, K. J., Emdin, C. A., Haas, M. E., Wang, M., Hindy, G., Ellinor, P. T., Kathiresan, S., Khera, A. v, & Aragam, K. G. (2022). Association of Habitual Alcohol Intake With Risk of Cardiovascular Disease.JAMA Network Open, 5(3), e223849–e223849.
- Kloner, R. A., & Rezkalla, S. H. (2007). To Drink or Not to Drink? That Is the Question.Circulation, 116(11), 1306–1317.
- Andersson, C., Schou, M., Gustafsson, F., & Torp-Pedersen, C. (2022). Alcohol Intake in Patients With Cardiomyopathy and Heart Failure: Consensus and Controversy.Circulation: Heart Failure, 0(0), 10.1161/CIRCHEARTFAILURE.121.009459.
- The abstract ‘Moderate alcohol consumption is associated with progression of left ventricular dysfunction in a European stage B heart failure population’ will be presented during the session ‘Heart failure is a complex syndrome: look at comorbidities’ which takes place on 22 May at 09:40 CEST at Moderated ePoster 1.
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”
 You might want to check out Vascular Discovery 2022, a 2 ½-day meeting, which is sponsored by the Council on Arteriosclerosis, Thrombosis and Vascular Biology, the Peripheral Vascular Disease Council, and the Council on Genomic and Precision Medicine, in cooperation with and the Society for Vascular Surgery’s Vascular Research Initiatives Conference (Flyer on the right).
You might want to check out Vascular Discovery 2022, a 2 ½-day meeting, which is sponsored by the Council on Arteriosclerosis, Thrombosis and Vascular Biology, the Peripheral Vascular Disease Council, and the Council on Genomic and Precision Medicine, in cooperation with and the Society for Vascular Surgery’s Vascular Research Initiatives Conference (Flyer on the right).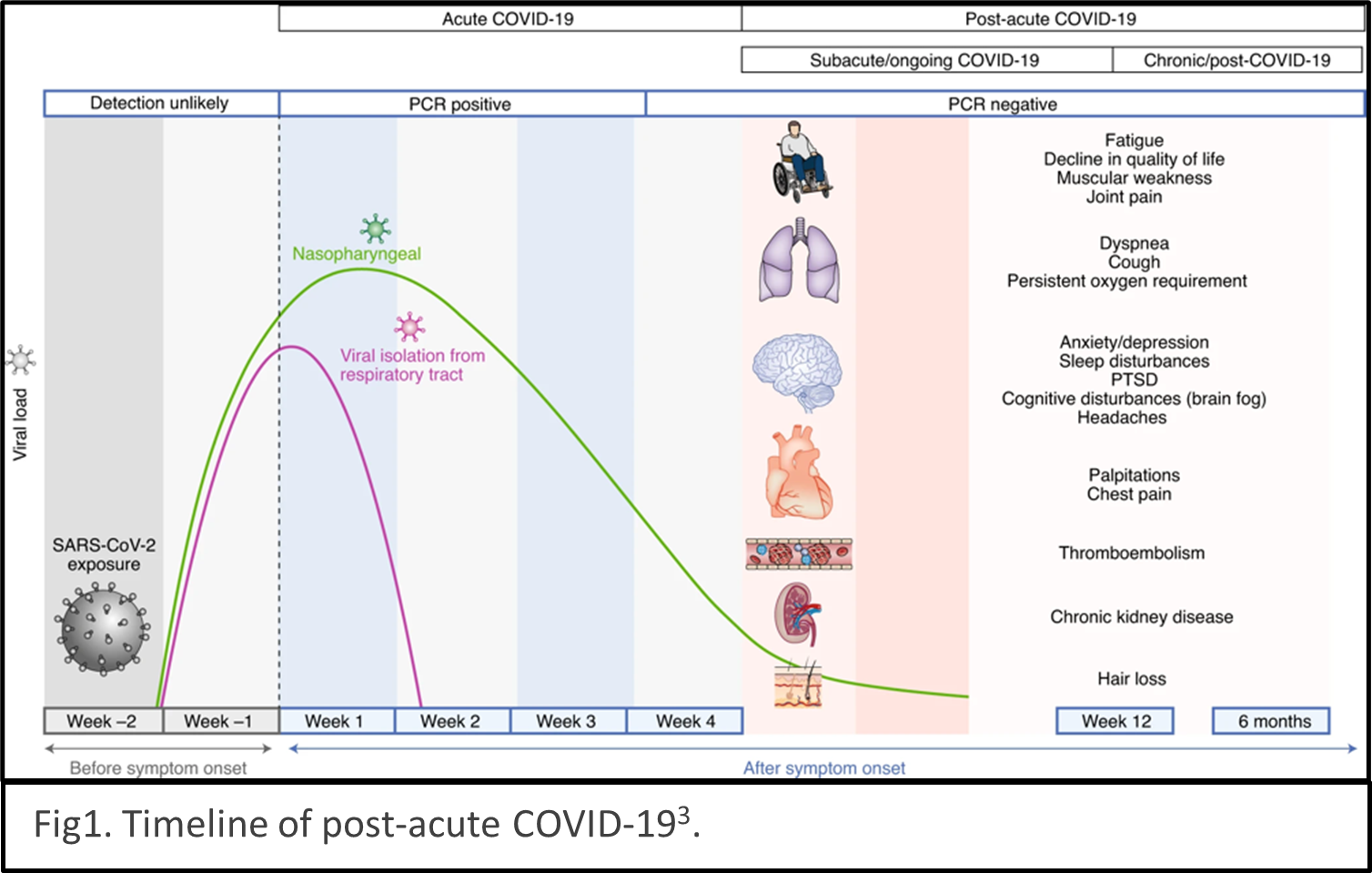 describes the condition as sequelae that extend beyond four weeks after initial infection1. The timeline of post-acute COVID-19 shows as Fig1. The list of common symptoms of post-COVID conditions is growing. Symptoms which people commonly report include difficulty breathing, fatigue, brain fog, cough, chest/stomach pain, headache, heart palpitations, muscle pain, diarrhea, sleep problems, fever, lightheadedness, rash, mood changes, changes in smell or taste, and changes in menstrual period cycles2,3. The challenges of diagnosing long COVID are multiple layers. The social isolation resulting from pandemic prevention measures can cause mental health stress such as depression, anxiety, and mood changes. Complications of pre-existing conditions may unmask after COVID infections.
describes the condition as sequelae that extend beyond four weeks after initial infection1. The timeline of post-acute COVID-19 shows as Fig1. The list of common symptoms of post-COVID conditions is growing. Symptoms which people commonly report include difficulty breathing, fatigue, brain fog, cough, chest/stomach pain, headache, heart palpitations, muscle pain, diarrhea, sleep problems, fever, lightheadedness, rash, mood changes, changes in smell or taste, and changes in menstrual period cycles2,3. The challenges of diagnosing long COVID are multiple layers. The social isolation resulting from pandemic prevention measures can cause mental health stress such as depression, anxiety, and mood changes. Complications of pre-existing conditions may unmask after COVID infections.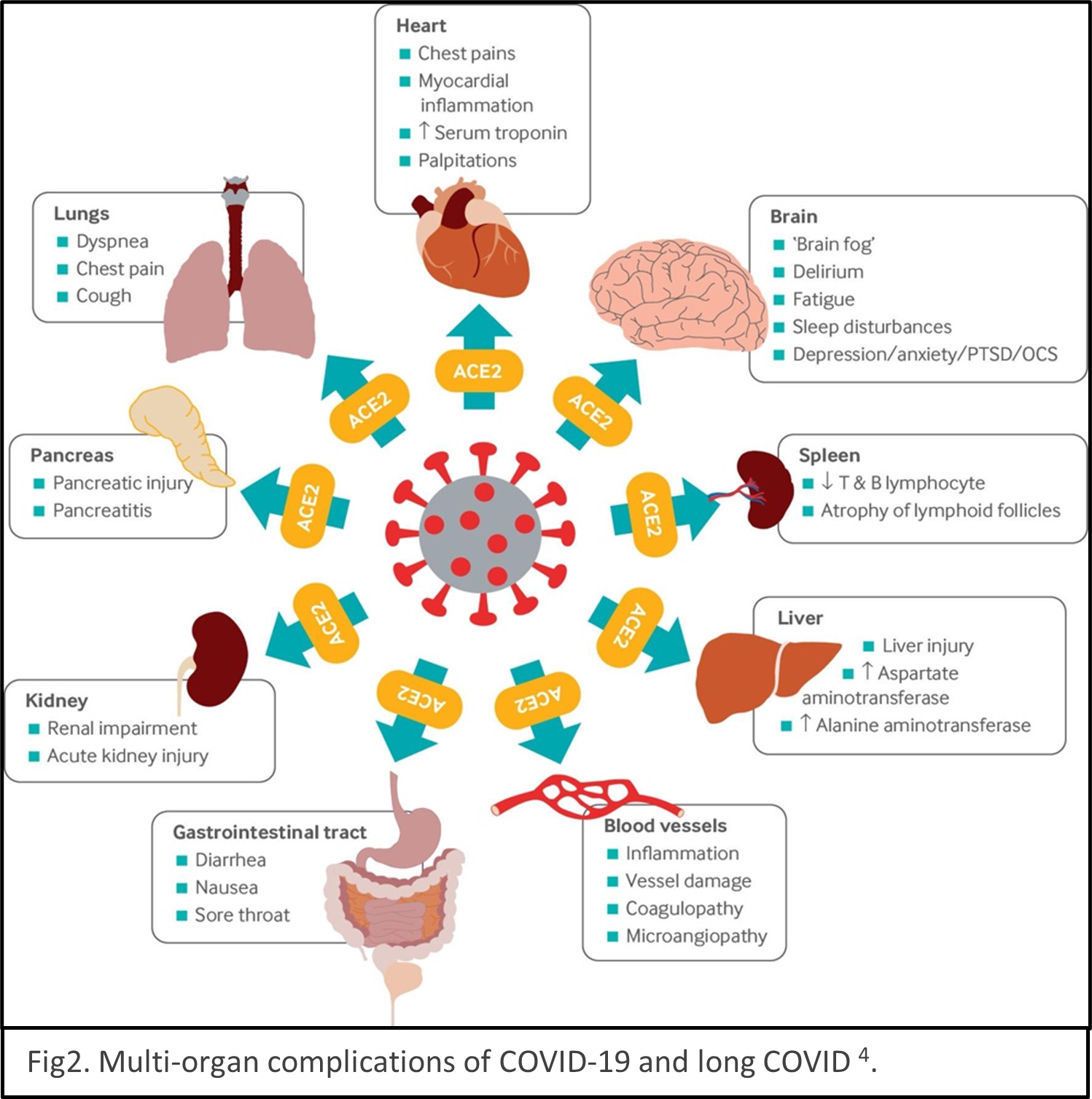 Reinfection of COVID could be mistaken as persistent symptoms. Multiple organs are reported being the victims of SARS-CoV-2 infection, for example, lungs, heart, brain, kidney, spleen, liver and the cardiovascular systems4 (Fig2). Some people have severe illness with COVID experience combinations of multiorgan effects or autoimmune conditions with symptoms lasting for weeks or months after initial infection. Long COVID is a serious concern. We just begin to understand it, and the path to be able to treat it with ease is winding.
Reinfection of COVID could be mistaken as persistent symptoms. Multiple organs are reported being the victims of SARS-CoV-2 infection, for example, lungs, heart, brain, kidney, spleen, liver and the cardiovascular systems4 (Fig2). Some people have severe illness with COVID experience combinations of multiorgan effects or autoimmune conditions with symptoms lasting for weeks or months after initial infection. Long COVID is a serious concern. We just begin to understand it, and the path to be able to treat it with ease is winding.
 unignorable. From the latest discoveries of epigenetics studies, results suggest that not only mother’s CVH can affect babies’ CVH, father’s CVH could potentially possess certain influences as well4.
unignorable. From the latest discoveries of epigenetics studies, results suggest that not only mother’s CVH can affect babies’ CVH, father’s CVH could potentially possess certain influences as well4.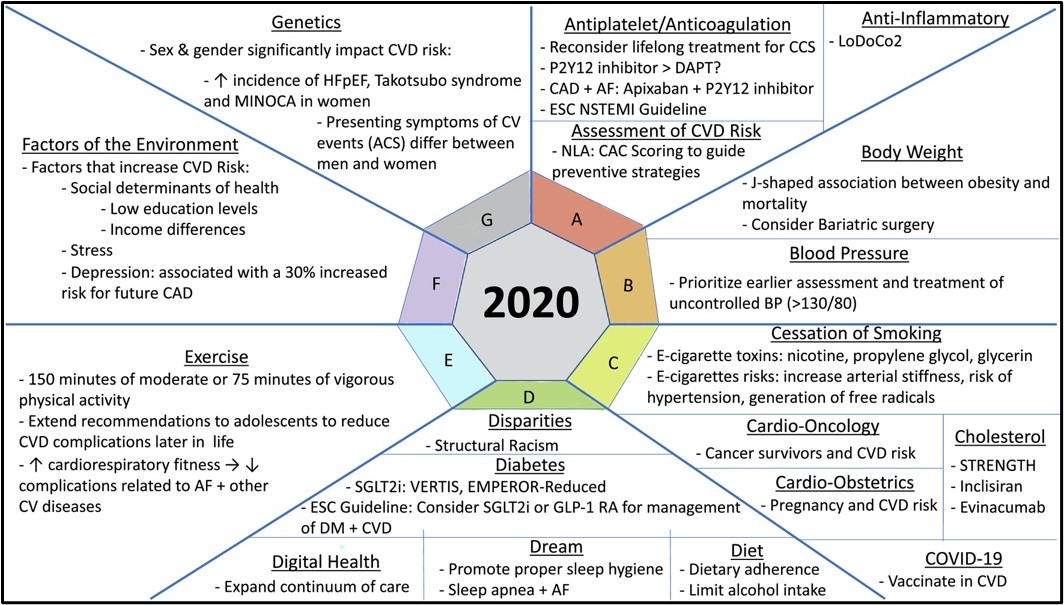 To improve quality of life in ageing population, other symptoms of ageing including physiological function decline start to capture scientific community’s attention. In AHA Scientific Sessions 2021, a panel of experts and professionals in the field talked about novel strategies to promote healthy vascular aging.
To improve quality of life in ageing population, other symptoms of ageing including physiological function decline start to capture scientific community’s attention. In AHA Scientific Sessions 2021, a panel of experts and professionals in the field talked about novel strategies to promote healthy vascular aging.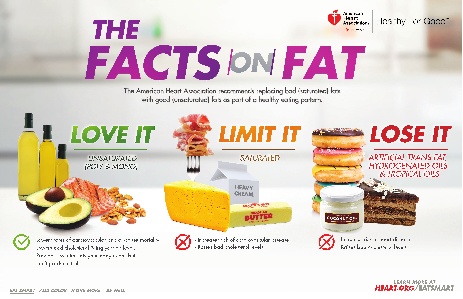
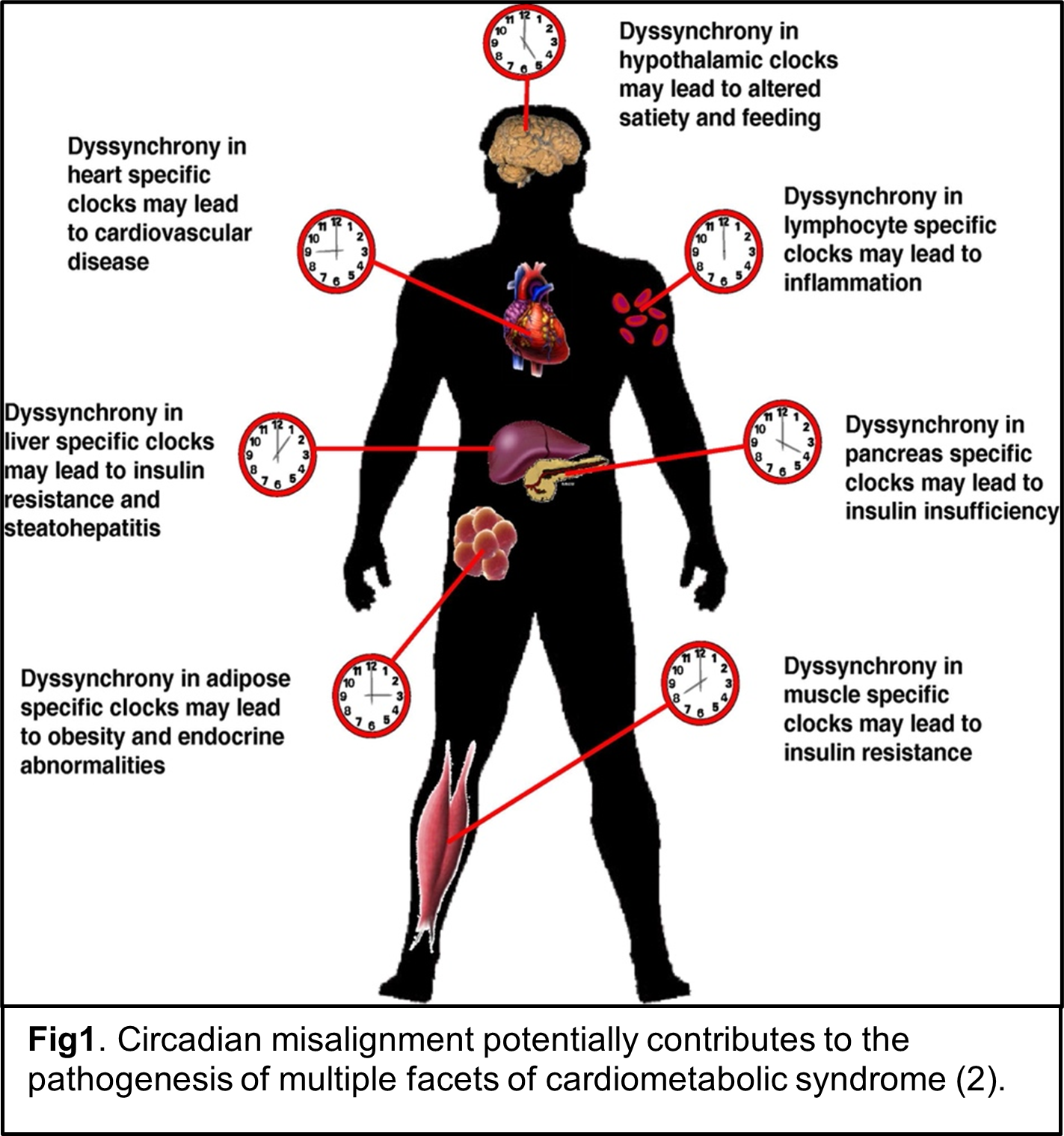
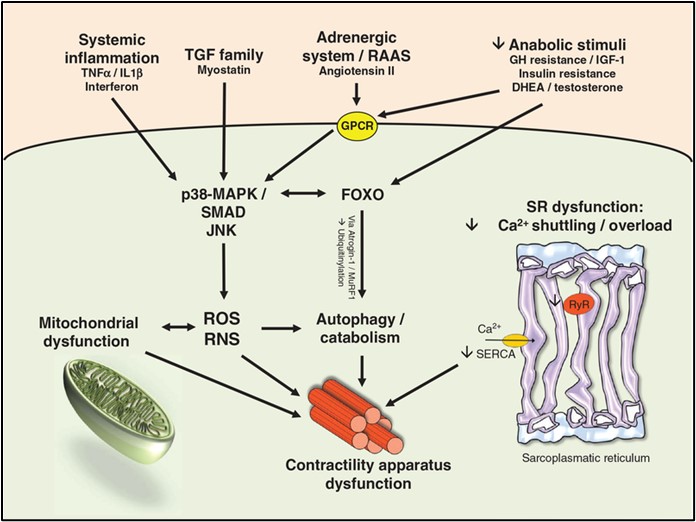 As we know, skeletal muscle mass decreases during the aging process, while cardiometabolic health often declines. A recently published epidemiology study investigated the relationship between skeletal muscle mass and cardiovascular disease in a group of adults (3042 people) without pre-existing cardiovascular risk in a 10-year follow-up study, ATTICA1. After adjusting for various confounders, this study showed a significant inverse association between skeletal muscle mass and cardiovascular incidence (HR 0.06, 95% CI 0.005 to 0.78). Moreover, it showed that people in the highest skeletal muscle mass group had 81% lower risk for a cardiovascular event. The results are quite intriguing. Does decreased skeletal muscle mass contribute to poor heart health or does a failing heart cause muscle mass decrease? It’s hard to figure out the cause and effect without understanding the relationship between skeletal muscle and the heart.
As we know, skeletal muscle mass decreases during the aging process, while cardiometabolic health often declines. A recently published epidemiology study investigated the relationship between skeletal muscle mass and cardiovascular disease in a group of adults (3042 people) without pre-existing cardiovascular risk in a 10-year follow-up study, ATTICA1. After adjusting for various confounders, this study showed a significant inverse association between skeletal muscle mass and cardiovascular incidence (HR 0.06, 95% CI 0.005 to 0.78). Moreover, it showed that people in the highest skeletal muscle mass group had 81% lower risk for a cardiovascular event. The results are quite intriguing. Does decreased skeletal muscle mass contribute to poor heart health or does a failing heart cause muscle mass decrease? It’s hard to figure out the cause and effect without understanding the relationship between skeletal muscle and the heart.