Near the End, and Preparing for a New Beginning
You’ve finally hit that point, where “comps” (comprehensive exams) has been completed. You passed. Now all you have to do is collect data, write it up and present it to your committee. The next challenge is figuring out the time to present the data you collected for the dissertation or thesis. Not to consider the biggest challenge of collecting data that is quality and timely. Thus, there is a few things to consider that might help streamline the PhD journey, or any similar terminal degree.
Thesis/Dissertation Tips
These tips need the context of a “best dissertation/thesis is a done dissertation/thesis”.
- Start coming up with ideas for your dissertation/thesis. The ideas evolve, be open to that. Discuss not only with potentially faculty, but also your friends and even family.
- Develop a rapport with all the faculty, feel out who may suit you and your journey the best. There is a fit that is needed on both the mentoring and mentee sides of the journey.
- Set expectations for yourself and then for your direct report or mentor. This will help ensure efficiency. The mentor has likely been in your shoes before, so he or she may view the initiative and eagerness as a positive.
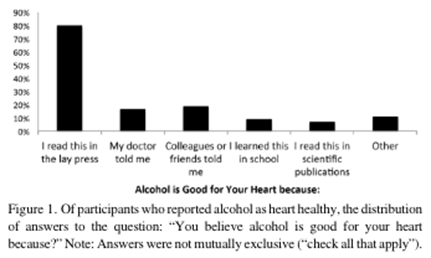
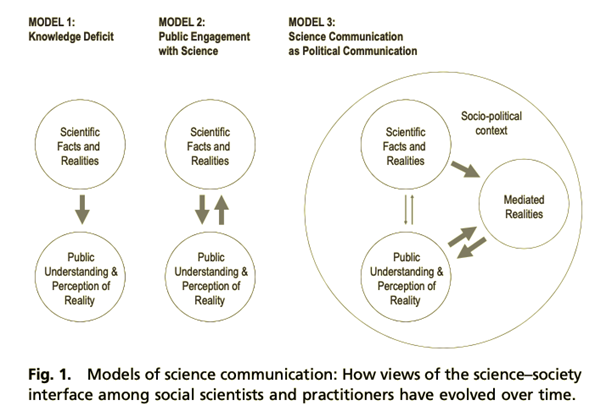
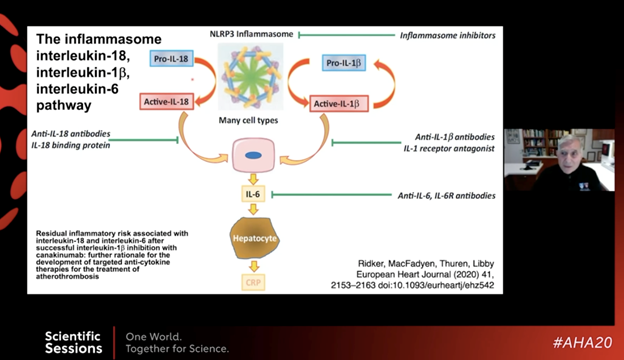
- At the same time learn to establish a balance between work and your life. Talk to your mentor about this, he or she likely has valuable input. This is important because the majority of graduate students experiencing anxiety and or depression did not agree with the idea of their advisor being as asset to their career (shown in Figure 1) (Evans et al., 2018).
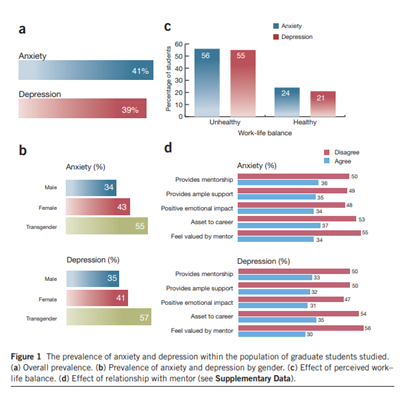
Figure 1. This figure highlights the graduate students and their experience of depression and anxiety as well as input related to perceived mentorship.
.https://doi.org/10.1038/nbt.4089.
- Make sure to back-up all your work. Back it up in more than one spot as well.
- It is never too early to start drafting up or writing down and organizing your ideas and concepts.
- Two sections that you really can get a jump on are the introduction and methods types of sections (Wyllie, 2021).
Future Investigator Tips:
On top of completing the thesis/dissertation, you should really be applying to jobs and considering what would be the next best step for you as a researcher. Dr. Douglas Seals published a very informative manuscript titled “The Academic Biomedical Research Laboratory as a “Small Business”. He provides a perspective that shows biomedical research laboratories providing services to external organizations (Seals, 2021). These services include:
“ -..manuscripts submitted for publication to scientific journals, grant applications submitted to biomedical research funding agencies; and abstracts submitted to professional organizations for presentations” (Seals, 2021).
Dr. Seals viewpoint manuscript is valuable because it highlights the need for developing a network. You learn about the future timelines and the associated potential hurdles. Furthermore, it will help address the a new type of balance, completing the work that you have obtained funding for, and beginning new work from ideas you have formulated. Beyond understanding the dynamics of a laboratory as a small business, developing yourself as a good writer will be something that continues, and a standard that should be set high for yourself.
- Find a skill set you would like grow with over time
- Look potentially broadening your network.
- Understand the importance of treating a lab like a small business.
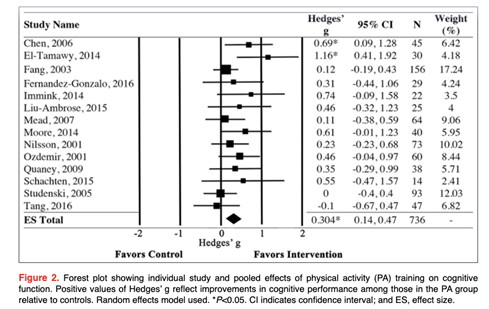
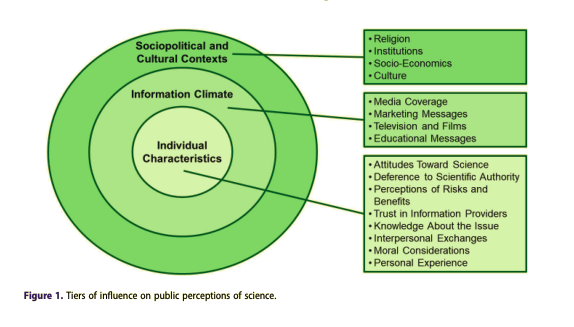
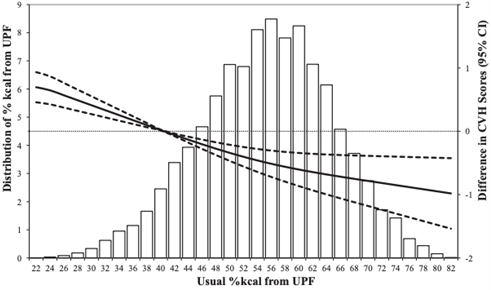
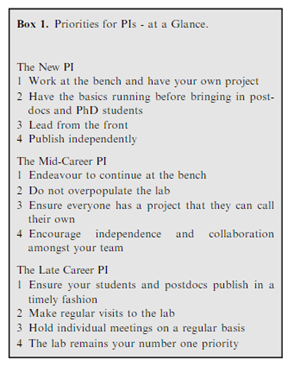
Below in Figure 2, shows what would be the priorities as a PI through a career. Understanding the frame-work over time can help you determine where you are and where you would like to be as an independent researcher. One of the skills that will need development, will be motivating a variety of people in a variety of ways (Banks, 2021).
https://febs.onlinelibrary.wiley.com/doi/epdf/10.1111/febs.15755
Finally, do your best to continue to find feedback from quality people with the network you established. Research is a process not only for sample and/or population studied, but for you and your development as an independent investigator. Develop patience and diligence.
Reference
Banks, L. (2021). Words of Advice: How to be a good Principal Investigator. The FEBS Journal, 288(13), 3973–3977. https://doi.org/10.1111/febs.15755
Evans, N. R., Shahrokni, R. O., Ferriday, D., Potter, C., Jebb, S. A., Brunstrom, J. M., & Rogers, P. J. (2018). Enhancing meal enjoyment: Evaluating the effects of flavour intensity and hedonic labelling. Appetite, 130, 304. https://doi.org/10.1016/j.appet.2018.05.184
Seals, D. R. (2021). The Academic Biomedical Research Laboratory as a “Small Business.” Journal of Applied Physiology. https://doi.org/10.1152/japplphysiol.00233.2021
Wyllie, D. J. A. (2021). Thesis write-up and manuscript preparation: Related but distinct tasks. The Journal of Physiology, 599(11), 2771–2775. https://doi.org/10.1113/JP281665
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”