Haemostatics: Stephen Hales and the first direct measurement of blood pressure
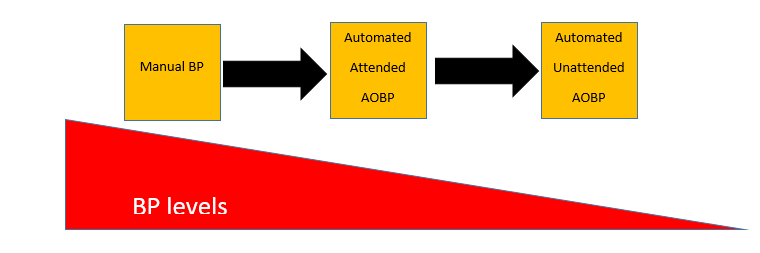
Blood pressure lowering medications are among some of the most effective and useful medications currently used in medicine. In 2017 the ACC/AHA released new guidance for the evaluation and management of high blood pressure in adults.1 This guidance outlines what is considered normal, elevated, and hypertension in adults.1 We now understand the great importance of blood pressure in health but this wasn’t always the case.
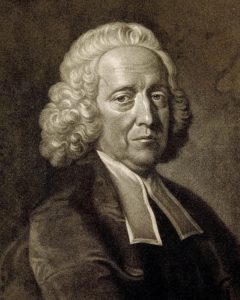
As far as we know, blood pressure was first mentioned by G. Harveo (1628) where he warned surgeons that blood could “jet out” of the artery.2 What I was interested in was the first measurement of blood pressure as we know it. That first measurement was done by Reverend Stephen Hales in 1733.2
I remember learning this during undergrad, and the image is striking. It is a picture of Hales and his associate with a horse laying on its side. They inserted a brass tube into the femoral artery connected to a glass tube running vertically out of the horse’s neck.3 The blood reached 8 feet 3 inches.4 Further work by Hales and others went on to describe blood pressures in different species and different vascular beds, but I haven’t been able to get the image of this horse out of my head.2
`

3(http://www.epi.umn.edu/cvdepi/wp-content/uploads/2011/05/Hales-Horse.jpg)
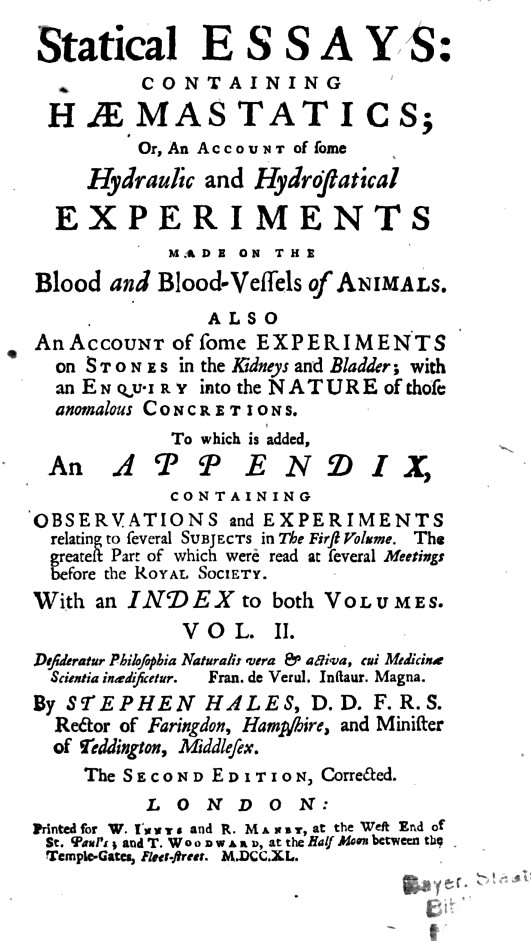
As my last post for the AHA Early Career Bloggers, I wanted to look into Stephen Hales. Who was he? Why did he do this experiment in the horse? And what else did he do? Hales was a Reverend in Middlesex who dabbled in many scientific pursuits. What I was interested in were those pertaining to the cardiovascular system. I went directly to the source: Statical Essays Containing Haemastatics.4
4 https://books.google.com/books?id=uDQ-AAAAcAAJ (eBook)
To get some context, this is what was thought about the cardiovascular system of arteries and veins at the time, “As an animal body consists not only of a wonderful texture of solid parts, but also of a large proportion of fluids, which are continually circulating and flowing, through and inimitable embroidery of blood vessels…it has, ever since the important discovery of the circulation of the blood, been looked upon as a matter well worth the inquiring into, to find the force and velocity with which these fluids are impelled…”4
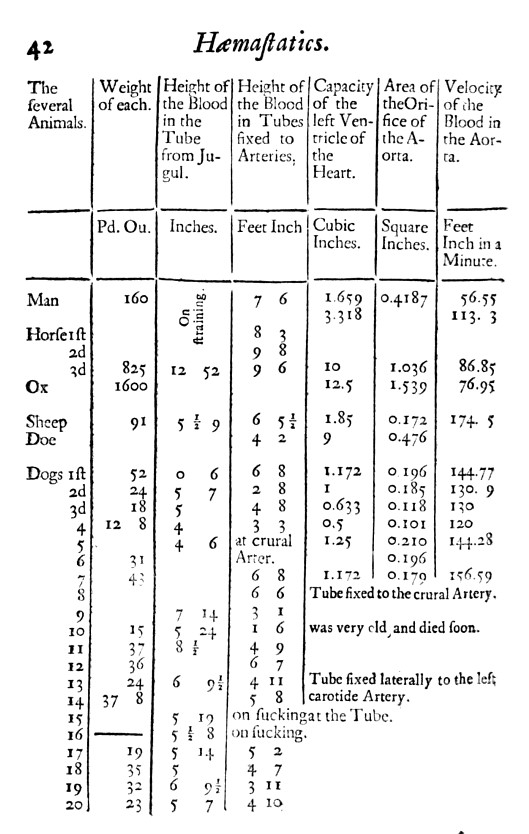
This book doesn’t have any illustrations, unfortunately, but there are descriptions of the many experiments Hales performed. He repeated his experiment on pressures in the horse several times. In fact, the famous image of Hales with the horse was from his 3rd horse experiment. Eventually Hales started collecting the blood and determining how much there was in addition to pouring wax into the empty heart to make a cast and determine the chamber volumes. He compiled this into a pair of tables. 4
4 https://books.google.com/books?id=uDQ-AAAAcAAJ (eBook)
Based on Hales’ measures, he calculated that “a quantity [of blood] equal to the dog’s weight, will pass through the heart in 11.9 minutes”. You’ll notice that Hales made calculations for “Man” but these were derived from data from the other animals and he never performed these experiments on humans.4
Stephen Hales contributed to science in many ways including in other fields. He is famous for inventing a ventilator that circulated air in ships, prisons, and mines which likely saved many lives. Hales had no medical training. He obtained a bachelors degree in divinity and a Master of Arts. Hales is a reminder that great discoveries can be made by anyone with a curious mind.5
4 https://books.google.com/books?id=uDQ-AAAAcAAJ (eBook)
Don’t forget to register for #Hypertension19 happening this September 5-8 in New Orleans!
References
- https://www.heart.org/-/media/data-import/downloadables/hypertension-guideline-highlights-flyer-ucm_497841.pdf
- The history of blood pressure measurement: from Hales to our days. V.A. Tsyrlin, M.G. Pliss, N.V. Kuzmenko. April 2016. Arterial Hypertension.
- http://www.epi.umn.edu/cvdepi/wp-content/uploads/2011/05/Hales-Horse.jpg (http://www.epi.umn.edu/cvdepi/essay/reverend-stephen-hales-on-blood-pressure/)
- Stephen Hales. Statical Essays Containing Haemastatics. (eBook: https://books.google.com/books?id=uDQ-AAAAcAAJ
- https://en.wikipedia.org/wiki/Stephen_Hales