Late-Breaking Science Presented at AHA20
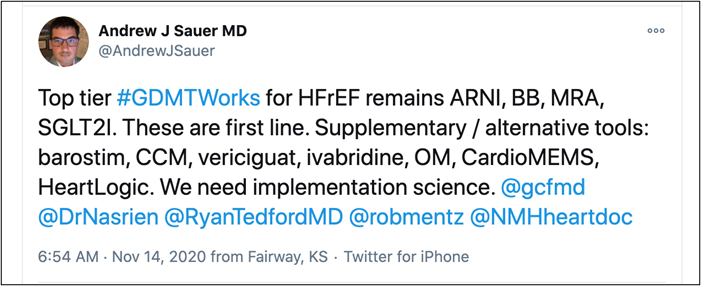
For this blog dedicated to #AHA20, I decided to put together a list of majority of American Heart Association (AHA) late-breaking study presentations at the 2020 Virtual AHA meeting from Day 1 to Day 3. So far, the late-breaking studies at AHA have covered a wide range of topics from heart failure, cardiovascular prevention focusing on a statin, newer LDL lowering therapies, Omge-3 fatty acid supplements, to polypills and imaging in women with MINOCA. Day 4 and Day 5 will cover multiple trials on atrial fibrillation, dual SGLT inhibitor, COVID, and Telemedicine.
Day 1
| Name | Trials | Study Population | Results | Conclusion |
| GALACTIC HF
cardiac myosin activator Omecamtiv Mecarbil In Chronic Heart Failure with Reduced Ejection Fraction: The Global Approach to Lowering Adverse Cardiac Outcomes Through Improving Contractility In Heart Failure |
Inclusion Criteria
Patients 18-85 years of age with CHF and NYHA class II, III, or IV symptoms LVEF ≤35% and pro-BNP ≥400 pg/ml
|
N= 8256
Follow up= 21.8 months Mean Age= 65 years Primary Outcome= cardiovascular death or CHF event
Mean LVEF: 27% ACEi/ARNI 87% Beta-blocker: 94% Aldactone 78% SGLT2iinhibitor: 2.5% |
Primary Outcome
37.0% of the omecamtiv mecarbil group compared with 39.1% of the placebo group (p = 0.03).
|
Among patients with HFrEF on GDMT, the selective cardiac myosin activator omecamtiv mecarbil was superior to placebo. It was associated with a reduction in the primary composite outcome; however, no benefit in outcomes of CV Death, all cause death, or change in KCCQ total symptoms score.
|
| AFFIRM-AHF
Ferric Carboxymaltose In Iron Deficient Patients Admitted for Acute Heart Failure
|
Inclusion Criteria
Hospitalization for CHF, and iron deficiency anemia- Serum ferritin <100 ng/ml or serum ferritin 100-299 ng/ml and transferrin saturation <20%, LVEF <50%
|
N= 1132
Follow up= 52 weeks Mean Age= 71 yrs Primary Outcome= total heart failure hospitalizations and cardiovascular death
|
Primary Outcome
52.5% of the ferric carboxymaltose group compared with 67.6% of the placebo group (p = 0.059).
|
Among patients with CHF with iron deficiency, intravenous ferric carboxymaltose was associated with a numerical reduction in total heart failure hospitalizations and cardiovascular death.
|
| VITAL
Omega-3 Fatty Acid and Vitamin D Supplementation In The Primary Prevention Of CV or cancer events |
Inclusion Criteria
Men >50 years or women >55 years without any known known cardiovascular disease or cancer |
N= 25,871
Follow up= 5.3 yrs Mean Age= 67.1 yrs Primary Outcome= CV death, nonfatal myocardial infarction (MI), or stroke
|
Primary Outcome
The primary CV outcome of CV death, nonfatal myocardial infarction (MI), or stroke, for vitamin D3 vs. placebo, was 3.1% vs. 3.2%, hazard ratio (HR) 0.97, 95% confidence interval (CI) 0.85-1.1, p = 0.69.
|
The results of this trial indicate that supplementation with either n–3 fatty acid at a dose of 1 g/day or vitamin D3 at a dose of 2000 IU/day was not effective in prevention of CV or cancer events
|
| TIPS-3
A Polypill For Primary Prevention Of Cardiovascular Disease In Intermediate Risk People: Results Of The International Polycap Study
|
Inclusion Criteria
Target CV disease (CVD) risk: >1.0%/year Men ≥50 years and women ≥55 years with an INTERHEART Risk Score (IHRS) of ≥10, or men and women ≥65 years with an IHRS of ≥5
|
N= 5713
Follow up= 4.6 yrs Mean Age= 63.9 yrs Primary Outcome= CV death, myocardial infarction (MI), stroke, heart failure (HF), cardiac arrest, revascularization |
Primary Outcome
Polypill vs placebo 4.4% vs. 5.5% (hazard ratio [HR] 0.79
|
Once-daily polypill (fixed-dose combination of simvastatin, atenolol, ramipril, HCTZ) was superior to placebo in reducing systolic BP, LDL-C, and nonfatal CV events at approximately 5 years among intermediate CV risk patients, mostly in Southeast Asia
|
Day 2-3
| Name | Trials | Topic of Interest | Hypothesis | Results |
| ALPHEUS
Ticagrelor Versus Clopidogrel In Elective Percutaneous Coronary Intervention
|
Inclusion Criteria
Patients undergoing nonemergent PCI At least one high-risk criteria: age >75 years, renal insufficiency, diabetes, body mass index >30 kg/m2, ACS in last year, LVEF <40% and/or prior episode of heart failure, multivessel disease, need for multiple stents, left main, bifurcation or complex PCI |
N= 1910
Follow up= 30 days Mean Age= 66 yrs Primary Outcome= |
Primary Outcome
MI ype 4a, 4b (stent thrombosis) or major myocardial injury at 48 hours
|
Among patients undergoing elective and planned PCI, ticagrelor loading was not superior to clopidogrel loading. Ticagrelor failed to reduce the incidence of periprocedural myocardial infarction. Major bleeding was also similar between the groups, although an increase in nuisance or minor bleeding with ticagrelor.
|
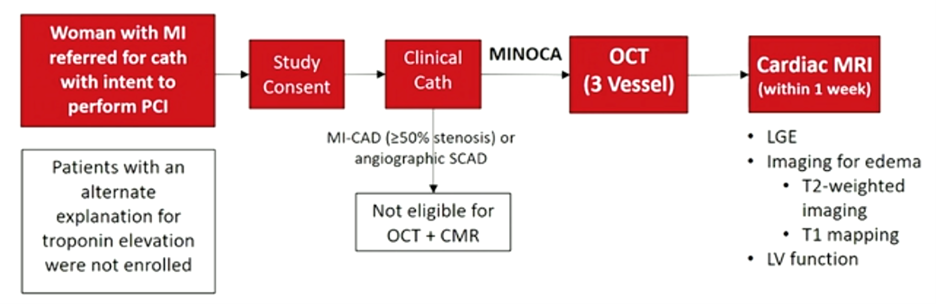
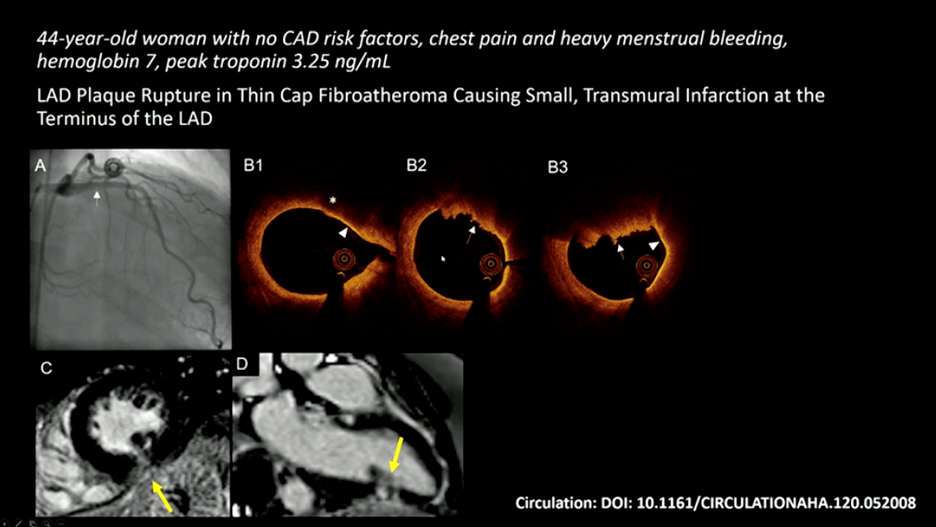
| HARP-MINOCA
Coronary OCT and Cardiac MRI to Determine Underlying Causes of Minoca in Women
|
Inclusion Criteria
prospective, multicenter, international, observational study, women with a clinical diagnosis of MI were enrolled |
N= 170
145 with OCT; 116 with CMR
|
46% pts with culprit lesion on OCT.
Abnormal CMR in 74% pts, ischemic pattern in 53%, nonischemic pattern in 20.7%,
|
Multi-modality imaging with coronary OCT and CMR identified potential mechanisms in 84.5% of women with a diagnosis of MINOCA, three-quarters of which were ischemic and one-quarter of which were non-ischemic, alternate diagnoses to MI
|
| RIVER
Rivaroxaban Versus Warfarin In Patients With Bioprosthetic Mitral Valves And Atrial Fibrillation Or Flutter: Primary Results From The RIVER Randomized Trial
|
Inclusion Criteria
≥18 years with bioprosthetic MV + AF/AFl without any contraindication to the AC
|
N= 1005
Follow up= 1 yr Mean Age= 59.3 yrs Primary Outcome= death, major adverse cardiac events, major bleeding Mean CHAD2vASC score= 2.6, HAS-Bled Score =1.6, 18% <3 months from MV surgery, 31% >5 yrs |
Primary Outcome
The mean time to the primary outcome for rivaroxaban vs. warfarin was 347.5 vs. 340.1 days (p < 0.0001 for noninferiority, p = 0.1 for superiority).
|
rivaroxaban is noninferior to warfarin for prevention of thromboembolic events among patients with AF/AFL and a bioprosthetic mitral valve. All strokes were lower with rivaroxaban.
|
| STRENGTH
Cardiovascular Outcomes with Omega-3 Carboxylic Acids (Epanova) In Patients With High Vascular Risk And Atherogenic Dyslipidemia
|
Inclusion Criteria
Statin-treated patients ≥18 yrs with or at high risk for cardiovascular disease and TG 180-500 mg/dl, HDL <42 mg/dl (men) or 47 mg/dl (women)
|
N= 13,078
Follow up= 42M Mean Age= 63Yrs Omega-3 CA Dose: 4 g/day Primary Outcome= cardiovascular death, MI, CVA, coronary revascularization, or hospitalization for unstable angina
|
Primary Outcome met in
12.0% of the omega-3 CA group compared with 12.2% of the placebo group (p = 0.84).
|
Among statin-treated patients with dyslipidemia and high cardiovascular risk, omega-3 CA was not superior compared to placebo.
|
| OMEMI
Effects Of N-3 Fatty Acid Supplements on Clinical Outcome After Myocardial Infarction In The Elderly: Results Of The Omemi Trial
|
Inclusion Criteria
Patients 70-82 years of age With Myocardial infarction 2-8 weeks prior to randomization
|
N=1,027
Follow up= 24M Mean Age= 74Yrs PUFA dose: 930g EPA+ 660g DHA Primary Outcome= all-cause death, nonfatal MI, revascularization, CVA, or hospitalization for heart failure
|
Primary Outcome
21.0% of the PUFA group compared with 19.8% of the placebo group (p = 0.62).
|
Among elderly patients with recent myocardial infarction, PUFA was not beneficial.
|
| SAMSON
A Three-arm N-of-1 Trial with Statin, Placebo And Tablet Free Periods, To Verify Side Effects And Identify Their Cause |
Inclusion Criteria
Patients with any adverse event within 2 weeks of starting a previous statin |
N= 60
Follow up= 12 months Primary Outcome: placebo symptoms divided by statin symptoms= termed nocebo ratio
|
Nocebo ratio was 0.90- meaning 90% of symptoms elicited by placebo tablets | Patients with previous adverse event to statin, 90% of the symptoms could be attributed to the nocebo effect |
|
EVINACUMAB The Efficacy and Safety Of angiopoietin-like 3 (ANGPTL3) inhibitor -Evinacumab In Patients With Refractory Hypercholesterolemia
|
Inclusion Criteria
Diagnosis of primary hypercholesterolemia (either heterozygous familial hypercholesterolemia [HeFH] or non-HeFH) with clinical atherosclerotic cardiovascular disease (ASCVD) with statin (± ezetimibe) at the maximum tolerated dose, PCSK9 inhibitor for at least 8 weeks with LDL-C ≥70 mg/dl or 100 mg/dl with or without clinical ASCVD, respectively
|
N= 160 (SC), 106 (IV)
Follow up= 16 weeks Mean Age= 54 years Primary Outcome= |
Primary Outcome
percent change in LDL-C from baseline
Phase II trial small and underpowered for clinical outcomes
|
Evinacumab is superior to placebo in reducing LDL-C among patients with refractory hypercholesterolemia despite being on statins, ezetimibe, and PCSK9 inhibitors (baseline LDL-C: ~150 mg/dl)
|
| SHORT-DAPT
One Month Dual Antiplatelet Therapy Followed By Aspirin Monotherapy After Drug Eluting Stent Implantation |
Inclusion Criteria
Patients ≥19 years of age undergoing PCI for stable or unstable ischemic heart disease AMI excluded
|
N= 3020
Follow up= 12 months Mean Age= 67 yrs Primary Outcome= cardiac death, nonfatal myocardial infarction, target-vessel revascularization, stroke, or major bleeding at 12 months
|
Primary Outcome
5.9% of the 1-month DAPT group compared with 6.5% of the 6- to 12-month DAPT group (p for noninferiority < 0.001; p for superiority = 0.48).
|
Among patients undergoing PCI for stable or unstable coronary artery disease, 1 month of DAPT was noninferior to 6-12 months of DAPT
|
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”