Highlights of “Not to Miss Sessions” at the #AHA20 Virtual Meeting!!
AHA20 virtual meeting has been packed by so many amazing sessions, covering all aspects of cardiovascular disease from basic science to clinical outcomes. I wanted to share some of the sessions “not to miss sessions” at AHA20 virtual meeting!!
Opening Session
Dr. Braunwald and Dr. Wenger, two of the legends in cardiology, took us back to history, structural racism, and correlated what we are living now during the pandemic and the social justice crisis to how it was when living in war!!!! Dr Harrington and Dr Yancy led a great discussion. Definitely, a very interesting talk that everyone should listen to!!
Structural Racism Session
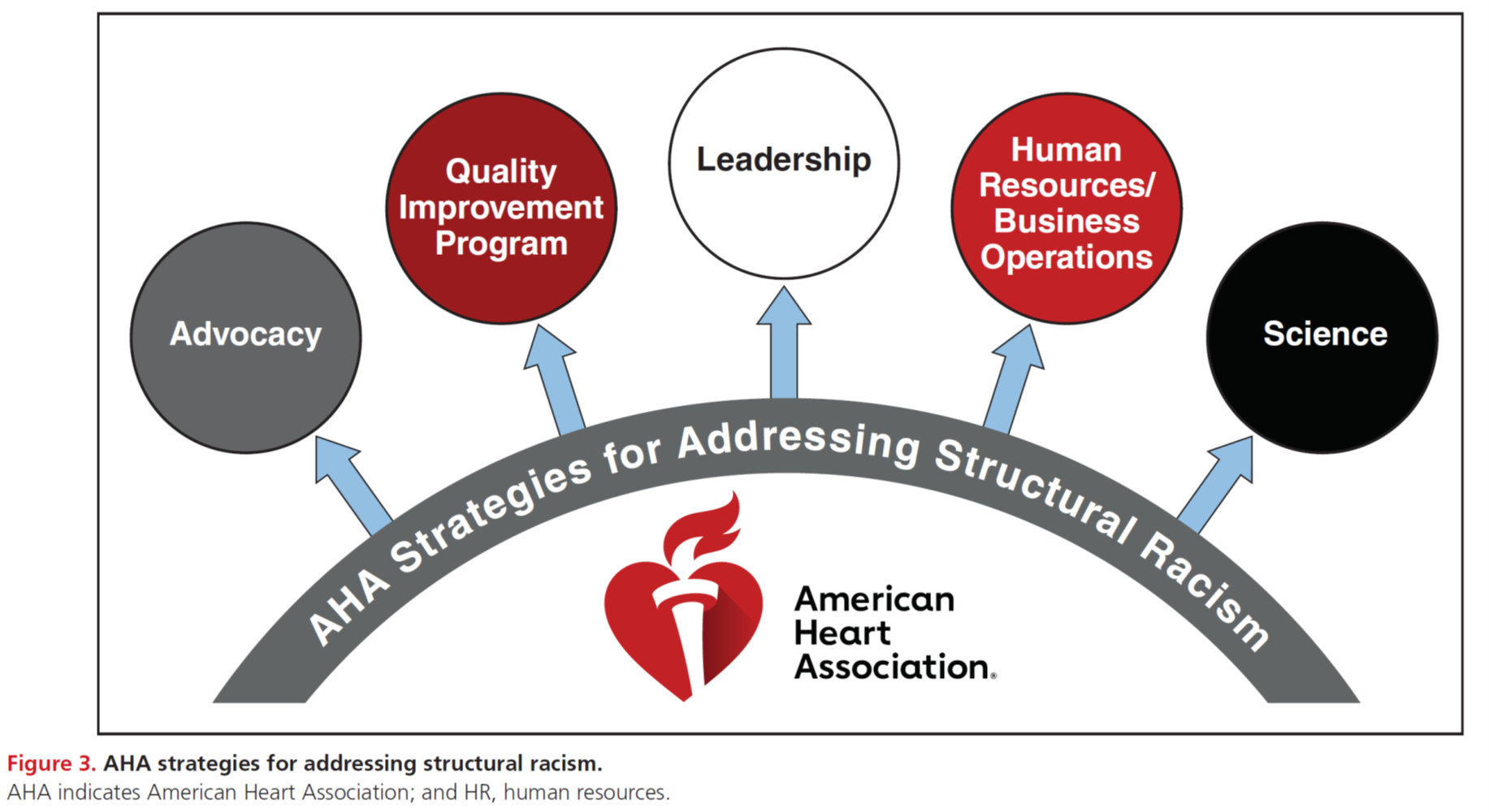
This is a novel yet a wonderful session at AHA20!!! It is part of AHA leadership commitment to equity, diversity, social justice in healthcare across the nation and the globe. There were several amazing discussions with experts and leaders in the field, sharing data on how structural racism can in fact affect the health of both healthcare employees and patients, calling for action to increase diversity and inclusion in leadership positions for minorities and women. If you missed this session, you should check out the on-demand portal and listen to it. Kudos to everyone involved in this and who made this happen!!
Presidential Session
This was an inspiring session by Dr. Elkind, MD, AHA President about his journey in neurology and science. This was followed by an amazing talk by Nancy Brown, AHA CEO, emphasizing the AHA vision on social equity, diversity, and inclusion in research, science, and access to health care. Then, we watched many inspiring women receiving distinguished AHA awards for their excellence in leadership and academic achievement. They all share the AHA’s vision and commitment to lead science in order to have comprehensive policies and unite team efforts for better healthcare for all as well as bridge the AHA’s visions into actual practice not only across the nation and also across the globe.
Late-Breaking Science and Meet the Trialist Sessions
There are late-breaking science sessions on multiple days on various sub-specialties of cardiovascular diseases, including preventive cardiology, resuscitation, heart failure, interventional cardiology, structural heart disease, electrophysiology, among other specialties. Later each day, there are sessions where you can meet the trialist, ask questions through Q&A side chat and you’ll hear their input on the trials they presented earlier in the day.
Move More and Dance Break Session
This is a fun session to motivate us to move more!! It was the first session of each day on AHA20 but you can watch it on-demand anytime whenever you want!!
#AHA20 is packed with so many great sessions for all sub-specialties in cardiology!! I look forward to AHA21, and hopefully, it will be an in-person meeting next year!!
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”