The Story of SGLT-2 Inhibitors
There were a lot of interesting presentations at the American Heart Association 2020 Scientific Sessions today. However, I found the most interesting was “But Wait, There are More Targets: SGLT-2 inhibitor…” by Dr. Marc Pfeffer. In his presentation, he discussed how did we end up using an antihyperglycemic drug (SGLT-2 inhibitors) in treating and preventing heart failure.
In 2008, the Food and drug administration (FDA) mandated that in order to approve glucose-lowering medications, cardiovascular safety should be established. Which was defined at the time as cardiovascular death, myocardial infarction, and stroke (heart failure was not included). Subsequently, all antihyperglycemic drugs were passing the bar when it comes to cardiovascular events. Until 2015, unexpectedly the EMPA-REG OUTCOME study showed that in patients with type 2 diabetes, empagliflozin had a lower rate of cardiovascular deaths, heart failure hospitalizations, and death from any cause.(1) Following this study, the endocrinologic and metabolic drugs advisory committee vote was split in regards to the impact of SGLT-2 inhibitors on cardiovascular outcomes. The final vote was 12 “Yes” vs 11 “No”, and as a result, the FDA concluded that SGLT-2 inhibitors reduced cardiovascular death.
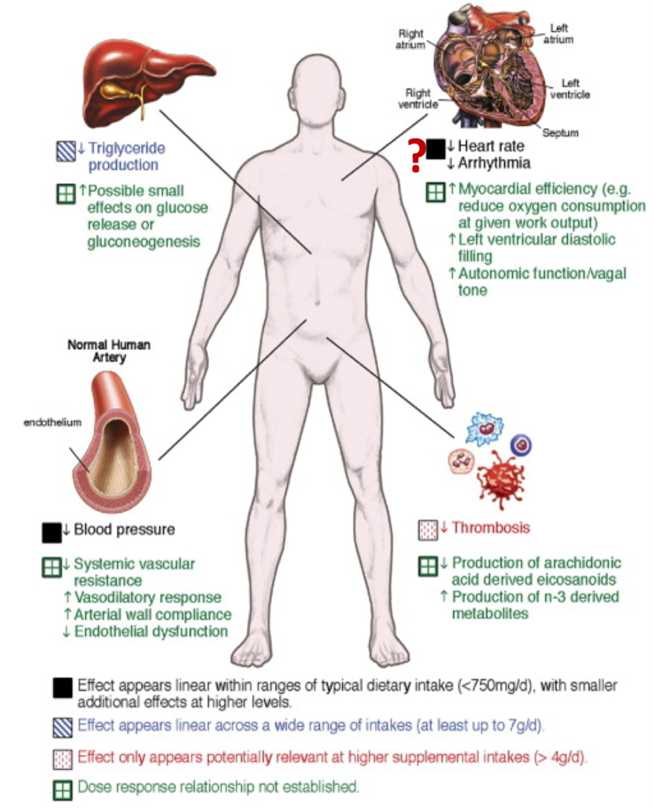
Afterward, EMPA-REG OUTCOME results were reproduced in several studies (CANVAS, DECLARE-TIMI). Most importantly, this effect was independent of HbA1c level. However, the population in the aforementioned studies were not predominantly heart failure patients. At this point, the cardiovascular community adopted the drug, and from 2017 to 2018 four large outcomes trials were launched (DAPA-HF, EMPEROR-Preserved, EMPEROR-Reduced and DELIVER) In 2019, DAPA showed that among patients with heart failure and a reduced ejection fraction, the risk of worsening heart failure or death from cardiovascular causes was lower among those who received dapagliflozin than among those who received placebo, regardless of the presence or absence of diabetes.(2) In 2020, EMPEROR-Reduced showed that among patients receiving recommended therapy for heart failure, those in the empagliflozin group had a lower risk of cardiovascular death or hospitalization for heart failure than those in the placebo group, regardless of the presence or absence of diabetes.(3) The previous findings were confirmed in a metanalysis that included both studies.(4) Although it is not very clear how SGLT2 inhibitors decrease cardiovascular events and heart failure, currently we have robust evidence proving its efficacy.
While many discoveries in medicine are incidental. I find the story of SGLT2 inhibitors as fascinating as other landmark accidental discoveries in medicine such as penicillin and warfarin. The moral of the story is always be observant and trust the data.
References:
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373(22):2117-28.
- McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381(21):1995-2008.
- Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-24.
- Zannad F, Ferreira JP, Pocock SJ, et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. The Lancet. 2020;396(10254):819-29.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”