If there is any silver lining to the horror that the COVID-19 pandemic has invoked, it is that this time has positioned us to take a critical look at systemic failures (or successes). Undoubtedly, the COVID-19 pandemic has magnified the institutionalized inequities that scholars have pointed to for decades as the root causes of health disparities. It is easy to point out the ways that we perceive the system has failed. It is much more sobering to consider that the system, in fact, has done exactly what it was designed to do. Rooted in structures as old as slavery and maintained by subsequent post-slavery policies aimed at maintaining white privilege well into the 20th century, structural racism represents a stronghold in American society hundreds of years in the making. As aptly drawn out by the AHA’s recent Presidential Advisory, these historical structures are tied to modern-day health outcomes. In a volley between ideals and policies, at face value, the effects of structural racism are easily disguised as individual behaviors, but we must be keen.
Structural racism (as defined by Lawrence and Keleher and employed by the advisory) is “the normalization and legitimization of an array of dynamics—historical, cultural, institutional, and interpersonal—that routinely advantage White people while producing cumulative and chronic adverse outcomes for people of color”. For example, Dr. David Williams pointed out during Saturday morning’s Structural Racism keynote that African American people earn $0.59 to every $1 earned by White people—a disparity that has existed since 1978. Moreover, regarding wealth—an even stronger predictor of health—African Americans have $0.10 to every $1 of wealth for White people. At every education level, race matters. Inequities reverberate through every social sector, including housing, the physical built environment, education systems, access to capital, and manifest in health outcomes. Indeed, “racism has produced a truly rigged system” by which the marginalized life and, ultimately, die.
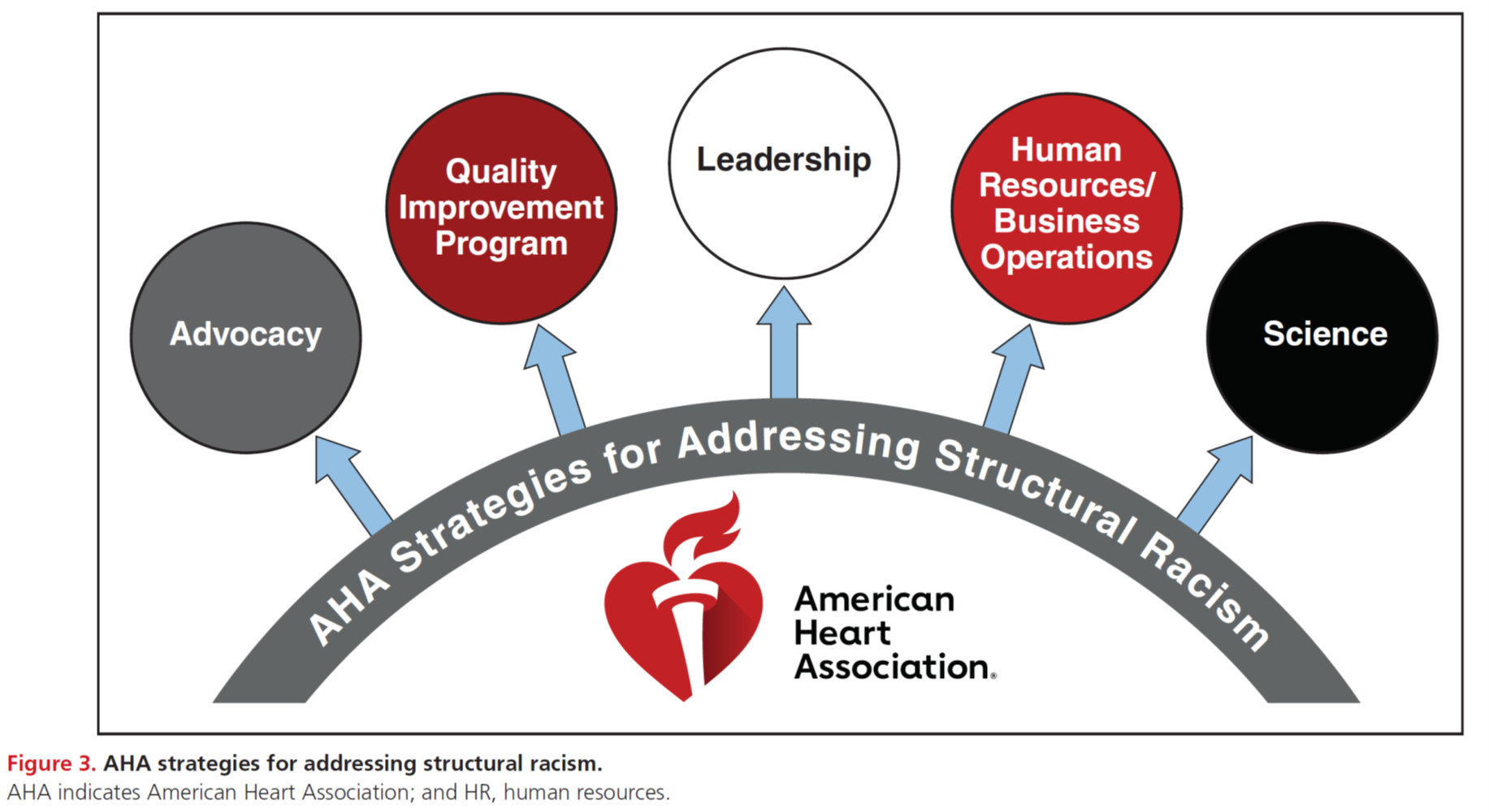
The AHA highlights its strategies to address structural racism, including advocacy, quality improvement, leadership, human resources/business operations, and, of course, science (see Figure 3, below). CEO Nancy Brown summarized the AHA’s role as one of “catalyst, convener, and collaborator”.
Assuming that “the long arc of the moral universe leans towards justice”, speakers during Tuesday’s press release and Saturday’s panel discussion emphasized that undoing structural racism should not fall solely on the shoulders of the communities that already bear the burden. Instead, the issue of achieving equity should be of interest to all. Further, Dr. Regina Benjamin emphasized that “allyship is more important than collaboration and that the privileged should work hand-in-hand” with the affected to dismantle these social ills. Solutions entail reforming the science and healthcare workforce, according to Dr. Lisa A. Cooper, to include more diversity, which leads to improved academic and workplace environments, organization academic excellence, improved access to care, and reductions in healthcare disparities. Others emphasized that we should evaluate our “investments as a moral template” and that real change may require “remapping entire curriculum and rethinking mentoring”.
In summary, as an early career scientist, I’m encouraged by the direction of this discussion. Though the length of my career in health disparities research pales in comparison to the giants on whose shoulders I stand, the attention to structural racism as a fundamental driver of health disparities feels like a long-awaited arrival. The path ahead will be even longer, but admission is the first step towards recovery. Moreover, I believe that all involved in the AHA’s thrust to acknowledge structural racism would agree with the African proverb,
“If you want to go fast, go alone. If you want to go far, go together.”
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”