Buzzword Alert! Artificial Intelligence – Just the Hype Man or a Genuine Showstopper?
Conversations of the utility and promise of machine learning (ML) and artificial intelligence (AI) permeate all fields of medicine, and cardiology is no exception. A quick search shows that 69 posters containing the keywords “machine learning” made it into AHA’s Scientific Sessions 2020. But is it for real? Will we really see a future in with ML/AI factors into all aspects of clinical care and in fact, re-write the script on how we care for patients?
Below is some of the discussion points and imperatives that stood out to me today from the “Hope or Hype? Artificial intelligence and Machine Learning in Imaging.” session at #AHA20 featuring thought leaders Drs. Marielle Scherrer-Crosbie, Alex Bratt, David Ouyang, Tessa Cook, Damini Dey, David Playford, and Geoffrey Rubin.
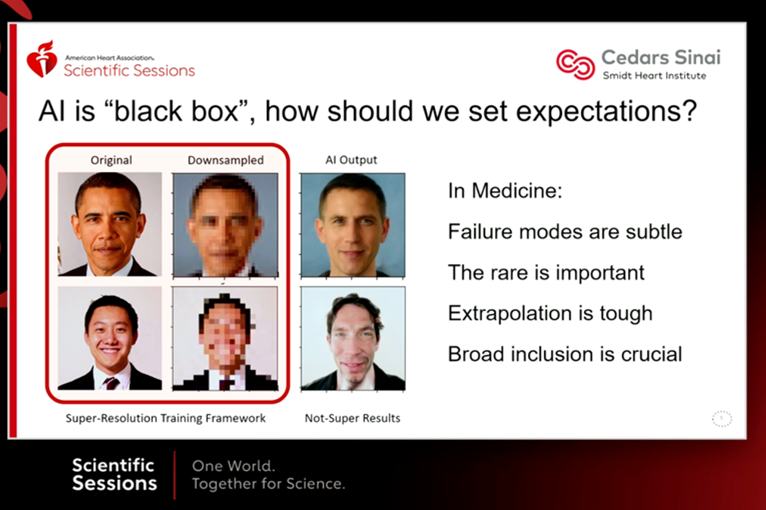
- While awe-inspiring in its ability to make inferences and predictions human beings often cannot themselves, we must be aware that ML/AI algorithms can recreate and reinforce the bias pre-existing in our society. We must fight this by knowing it is a possibility, screening for it, and training algorithms on datasets that are truly representative. As much of the political landscape and national conversation right now centers on structural racism and bias in America, it’s is prudent to understand how the models we create can perpetuate this.
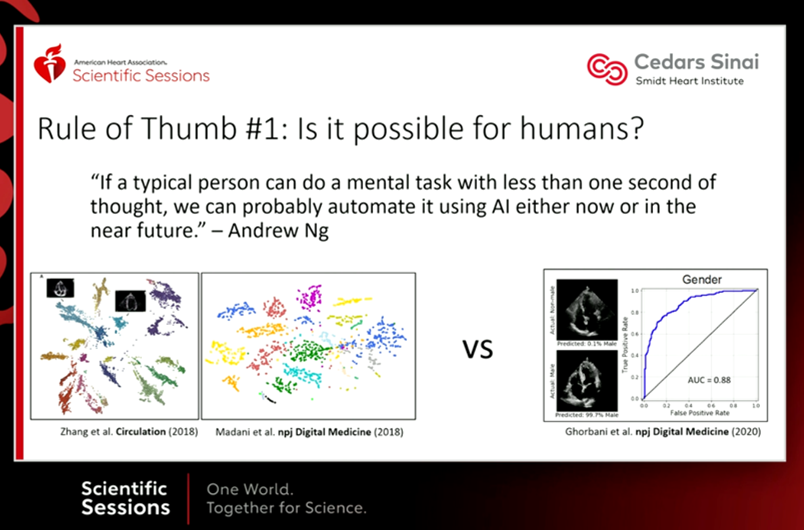
- Separate low hanging fruit from the unrealistic (at the moment) and consider the unrealistic tasks in the realm of discovery science. A quick rule of thumb provided by Dr. Ouyang, summarizing the words of Dr. Andrew Ng, first determines if it is possible for humans to do a task relatively quickly. If it is, we can probably automate it with AI now or in the near future.
- Scrutinize our data. How much do we trust it? High-quality data for ML/AI means broad, accurate, and plentiful. We need robust training labels, as free from subjectively as possible.
- How open is our data for inspection? Fields in computer science are far further along than medicine in deploying and improving ML/AI models because of open data sets and shared code, allowing groups to verify, tinker, and re-create to move the needle forward. Medical AI has not been so forthcoming.
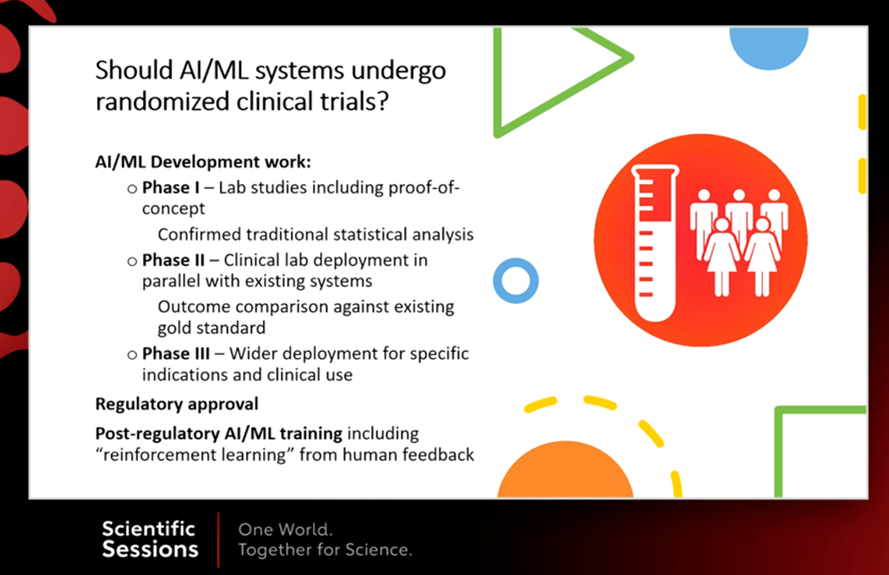
- As new technology is rapidly evolving and making it into the clinical space, we need to be responsible for mistakes. This means we need to assess not only our model performance before deploying but also the consequences of using the model in real life. This may require RCTs and to consider ML/AI algorithms like we consider new therapeutics.
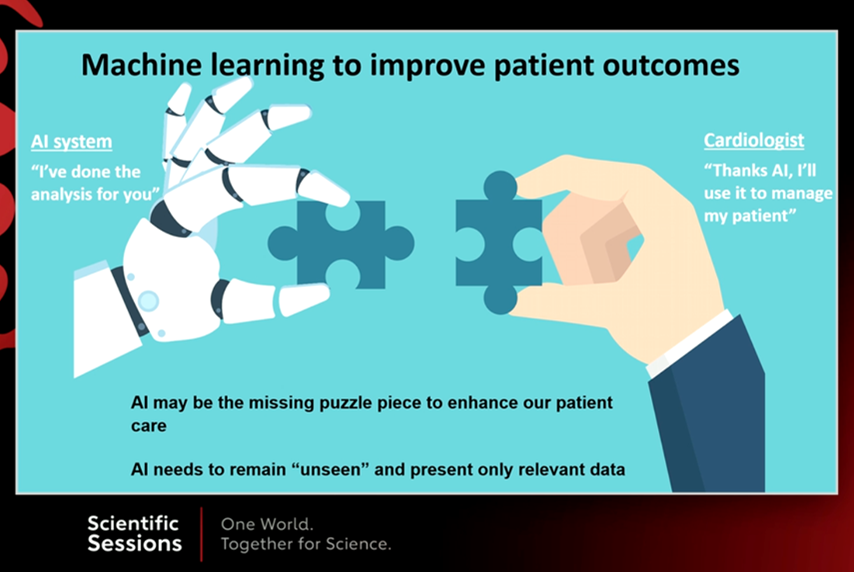
- What we really want is the AI running in the background saying “Hey, this task was automated and is now solved for you. Proceed as you see fit.” Humans and machines are in this shared space. The more we can integrate ML/AI to help us with tasks we are already doing, the better our results will be.
So where does this leave us? Most in our field believe ML/AI will play an important role in our future. Ideally, we will do it in a way that will make sure human intelligence is always paired with artificial intelligence to create a product neither of the two could be alone, will ensure our algorithms are free of bias and openly shared to allow for continuous improvement.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”