What Do We Know About the Future? The Digital Health Era
What do we know about the future? Although millions of possibilities come into mind, one thing is certain. One way or another, our lives are more and more dependent on computers and social media networks. How many of you check on your smartwatch or social media feeds more than once a day? I, for instance, am occasionally obsessed with my heart rate measurements and sleep patterns and constantly try to get a better understanding on how to optimize my own health. It’s very easy to get lost in trying to find the right kind of research from scientific journals. Most of the time people turn to social media to get ideas to make a healthcare decision. Study shows that 80% of internet users are looking specifically for health information1.
In today’s American Heart Association Scientific Sessions, a group of pioneers shares their insights in novel technologies for arrhythmia detection2 using big data to manage patient care systems. Dr. Leslie Saxon, of the University of Southern California Center for Body Computing, discussed the advancements of digital health, such as increased diversity of computer monitoring devices, increased data accessibility via the cloud, and novel digital biomarker identification. Particularly, using remote device follow-up improved 30-40% survival rate of patients after cardiac defibrillator implantation, according to a published clinical study (the ALTITUTE survival study)3. Another highlight from Dr. Leslie’s research, CORA, is a patient-facing, manufacturer-agnostic mobile application. CORA can help improve communications between patients and caregivers, visualize complex data in a simple way, and educate patients and caregivers about their health conditions.
Other advances in finding software solutions driven by big data collection are also critical in this digital era. An ongoing clinical study to determine if the Apple Watch and a heart health program can improve heart health outcomes, HEARTLINE, are recently launched in Feb 2020 with a collaboration between Johnson& Johnson and Apple (Clinical Trial NCT04276441).
Dr. Marco V. Perez from Stanford University talked out the recent developments of patient-acquired wearable technology, such as devices to monitor blood oxygen levels, glucose levels, and sleep rhythm. One of the challenges is potential data overload. Dr. Perez’s team implemented a machine learning algorism using a convolutional neural network to investigate 1.5 million ECG graphs from 500,000 patients collected from wearable devices. This artificial intelligence approach opens a new window with many possibilities in the health care systems and address novel research problems. Dr. Khaldoun G. Tarakji from Cleveland Clinic discussed how to use wearable devices to detect atrial fibrillation from a clinical practice perspective. He presented several case studies on using Apple watch to help diagnose and manage atrial fibrillation. In the field of telemedicine, Dr. Tarakji mentioned the advantages of using wearable devices to conduct virtual visits to improve patient care outcomes.
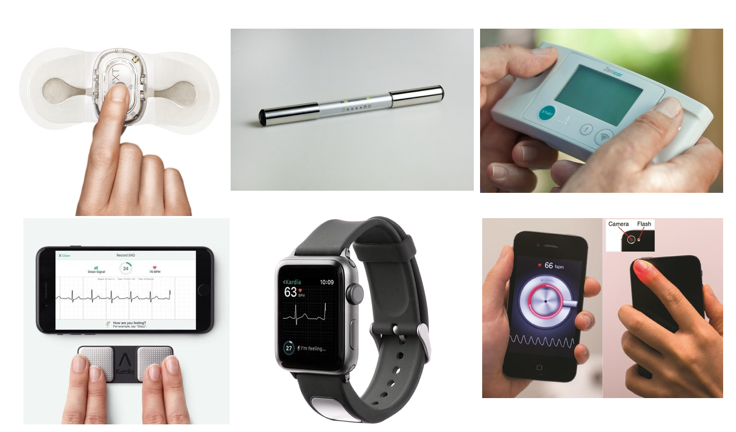
Figure 1: New technologies for the detection of atrial fibrillation 2
Despite apparent advantages of the application of wearable devices in the health care system, Dr. Paul D. Varosy from the University of Colorado discussed the challenges of using wearable devices regarding clinical, legal, cybersecurity, and ethical implications. The main questions are: How to fit data management into busy clinical practice? How to maintain financial sustainability? How to improve cybersecurity vulnerability? How to handle potential oversight? And who owns the data? These questions require continuing efforts from policy workers, researchers, doctors, and patients to work together to find solutions.
The new kid on the block: social media in the health care system. Dr. Janet K. Han from UCLA talked about the possibility of using social media to transform arrhythmia health care. Social media can make health information more accessible, engage patients better, provide valuable social and emotional supports4. Combining social media with big data with artificial intelligence and machine learning provides faster diagnosis and management5.
Wearable devices in combination with big data analyses in healthcare practices have a promising future. They are more accessible, engaging, and high payoff. Despite potential challenges, the era of digital health presents many possibilities and advantages in patients’ healthcare outcomes.
Reference
- Fox S. Profiles of Health Information Seekers. Pew Internet & American Life Project. 2011.
- Zungsontiporn N, Link MS. Newer technologies for detection of atrial fibrillation. BMJ (Online). 2018.
- Saxon LA, Hayes DL, Gilliam FR, Heidenreich PA, Day J, Seth M, Meyer TE, Jones PW, Boehmer JP. Long-term outcome after ICD and CRT implantation and influence of remote device follow-up: The ALTITUDE survival study. Circulation. 2010.
- Hawkins CM, DeLaO AJ, Hung C. Social Media and the Patient Experience. Journal of the American College of Radiology. 2016.
- Simonsen L, Gog JR, Olson D, Viboud C. Infectious disease surveillance in the big data era: Towards faster and locally relevant systems. Journal of Infectious Diseases. 2016.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”