What an end to the weekend! As Day 3 of AHA 2020 continues, there is already much to digest and discuss. From Late-Breaking Trials to specific programming for Fellows in Training and Early Career individuals, there was something for us all. My time was spent tuning in to informative discussions from leaders in the advanced heart failure world, and below I reflect on some of what stood out to me today.
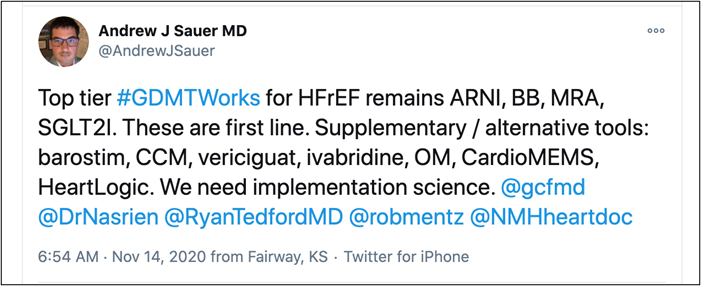
- Implementation science matters as Dr. Saurer shares with us on Twitter. As our armamentarium of GDMT grows, it will be key to figure out how best to get these medications prescribed to our patients in order to maximize therapy while minimizing side effects and managing cost. But how do we do that? What order should be prescribed our drugs in? What about devices? Is the same approach applies to all? There is an area primed for more research. What an exciting time to be in the heart failure space.
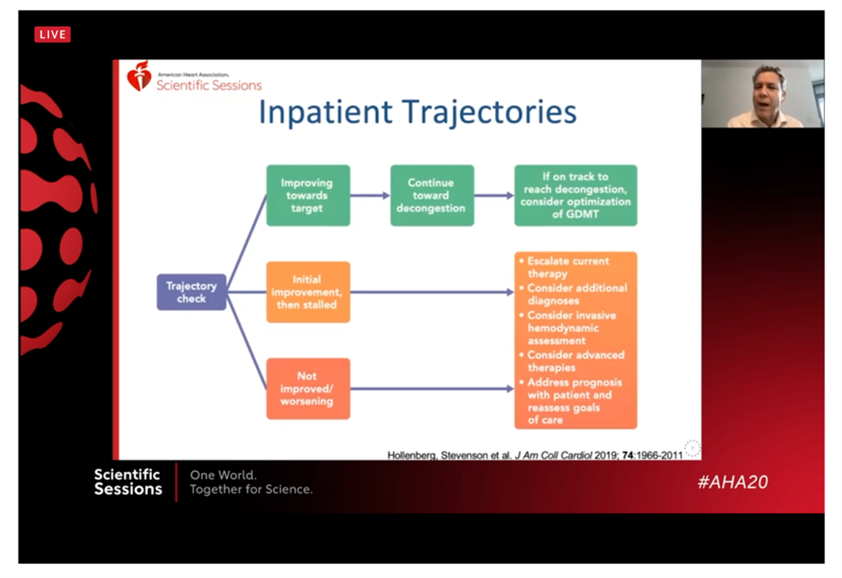
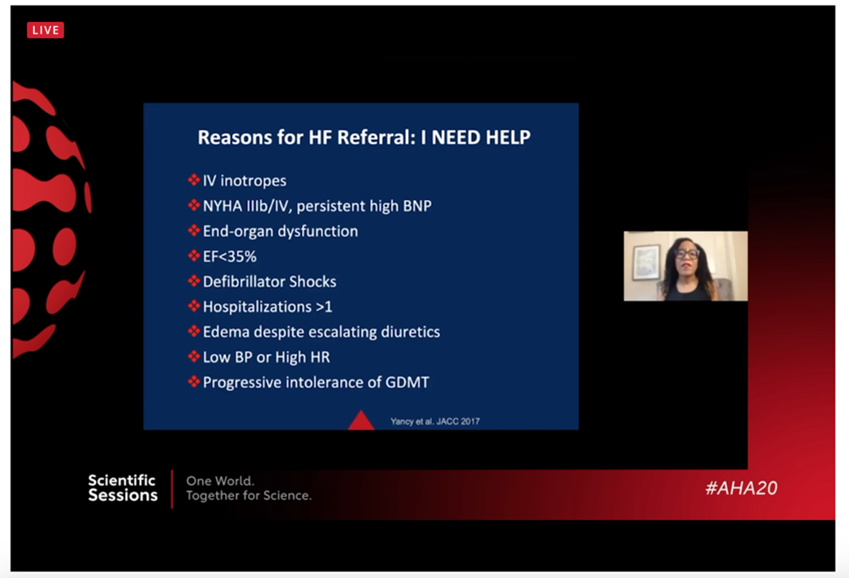
- Take note of the trajectory. It is important to be aware of and routinely reassess the trajectory of our patients with heart failure, both in the inpatient and outpatient setting, as discussed by Dr. Hollenberg. In our sickest patients, those with Stage D heart failure, we have the option of considering VAD or transplant as well as palliative care approaches including home inotropes, but patients are often flagged too late and no longer eligible for certain therapies. Use the “I NEED HELP” mnemonic to try and identify these patients early, as Dr. Breathett shares with us.
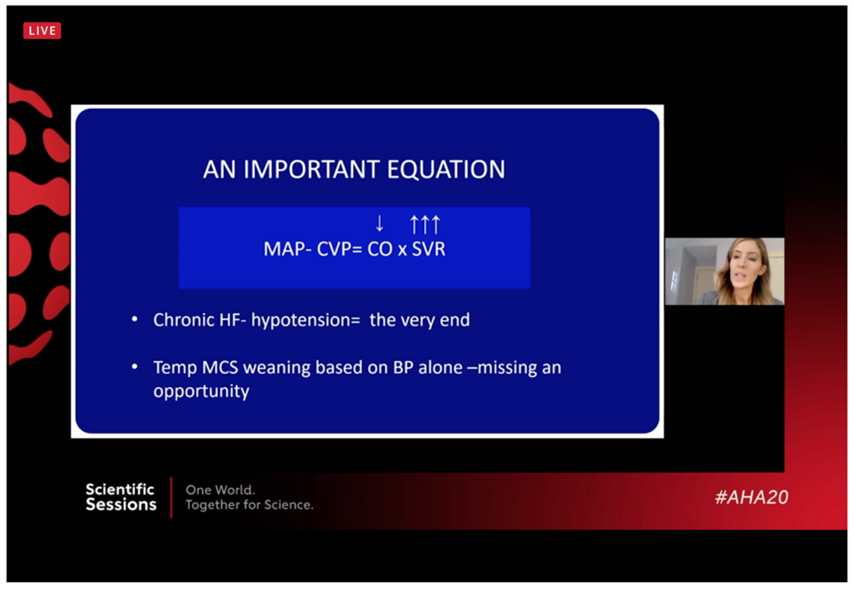
- Know when to escalate care. While it is not always crystal clear who needs a higher level of support, Dr. Cogswell gives us a clinical pearl: if your patient is hypotensive with heart failure, start to think about what is next, whether that is temporary support or a durable device or ultimately both. She gives an example of pausing an IABP and seeing if her patient becomes hypotensive in order to consider an Impella or LVAD, as opposed to adding more drips which may not ultimately be enough.
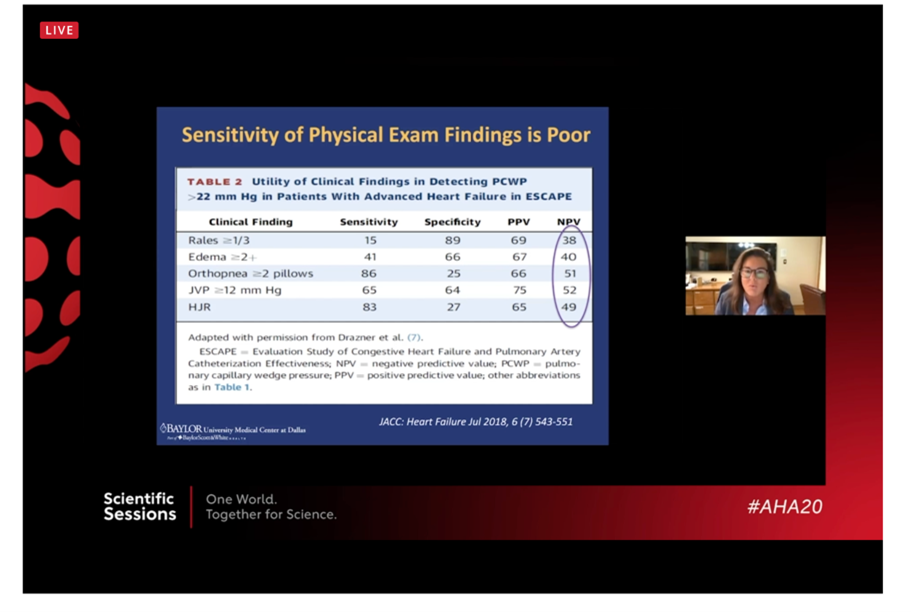
- #ReviveTheSwan! As eloquently and definitively stated by Dr. Hall, all patients with cardiogenic shock need a Swan-Ganz catheter. Our physical exam “just is not that good”. Care is improved by using invasive hemodynamics
- A civilized debate is possible! Despite the politics in our country as of late, today’s sessions clearly showed the civil, intellectual, informative debates are still possible in our society, and they are for the betterment of all involved! Kudos to all who gave us their time and wisdom today.
While the day is early and there is much yet to be seen, the teaching on Day 3 of AHA20 has already been fantastic.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”