Gestational Hypertension (GHTN) is defined as the new onset of systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg , on at least 2 occasions 4 hours apart , at or after 20 weeks of gestation in a previously normotensive woman . It is considered as one type of the major hypertensive disorders in pregnancy; which also includes Pre-eclampsia, eclampsia and chronic hypertension. [1]
Hypertensive disorders of pregnancy is one of the leading causes of maternal and perinatal mortality. It can complicate the pregnancy leading to multi-organ damage such as renal failure, liver failure, pulmonary edema, fetal growth retardation and cerebral symptoms. [1]
The main target in controlling the maternal BP readings is to reduce the risk of maternal stroke and heart failure. So we will talk briefly about the medications used during pregnancy that are considered safe to achieve this target.
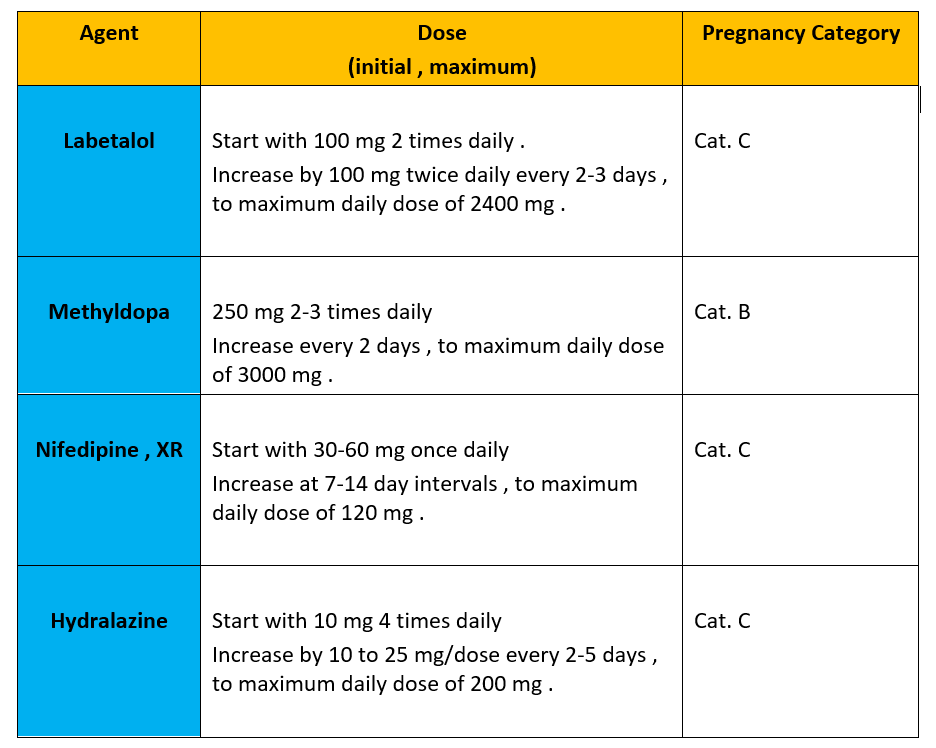
* First-line Oral Drugs used to treat NON-severe HTN in pregnancy , the choice among these agents is based on adverse effects , contra-indications , availability and patient preference : [2]
1-Beta-blockers :
The preferred drug in this class is Labetalol [3]. Metoprolol and pindolol are acceptable alternatives, provided that they are less well-studied In pregnancy [4].
2-Calcium Channel Blockers :
Nifedipine is the most widely used in pregnancy, preferred as intermediate- or extended-release formula [5]. Amlodipine can be used in early pregnancy, since it was not associated with increased risk of fetal malformations [6].
3-Methyldopa :
It is widely used in pregnancy due to its long term safety profile [7] .
4- Hydralazine :
The current available evidence does not support the use of Hydralazine as first line agent due to its adverse effects, reflex tachycardia and peripheral edema. So it’s preferred to be used as add-on therapy [8] .
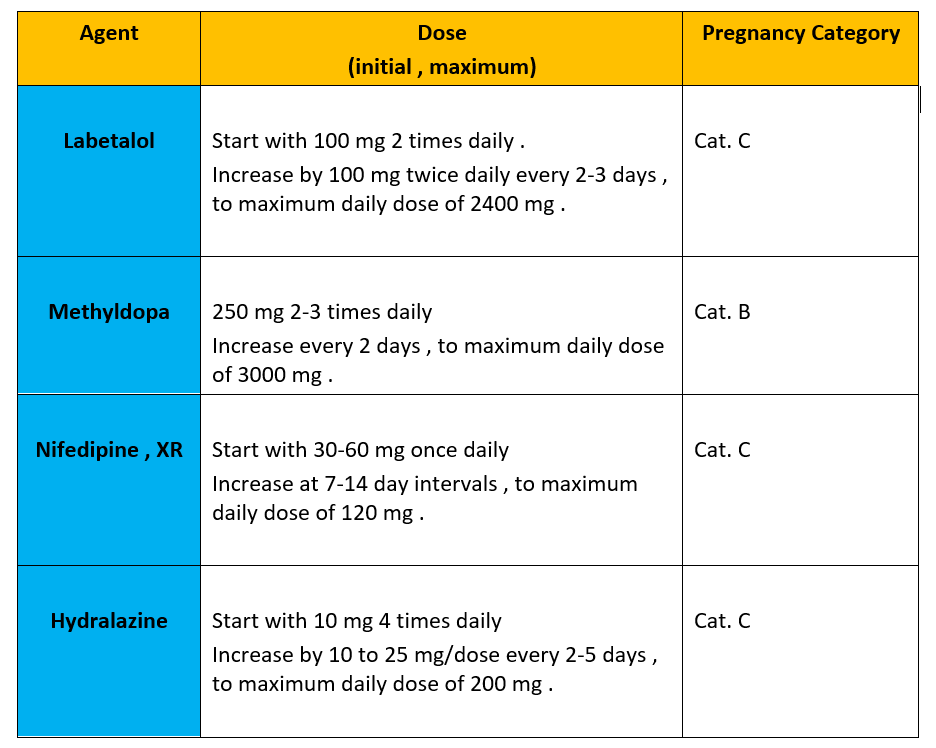
Table 1 : summary of drugs used in NON-severe GHTN in pregnancy
** Here are some Common anti-hypertensive Drugs to be AVOIDED in pregnancy; due to increased risk of congenital malformations : [9],[10]
- ACE inhibitors ( -pril , e.g : enalapril , lisinopril … etc )
- ARBs ( -sartan, e.g : valsartan , candesartan … etc )
- direct renin inhibitors ( e.g : Aliskiren )
- Mineralocorticoid receptor antagonists ( such spironolactone , amiloride )
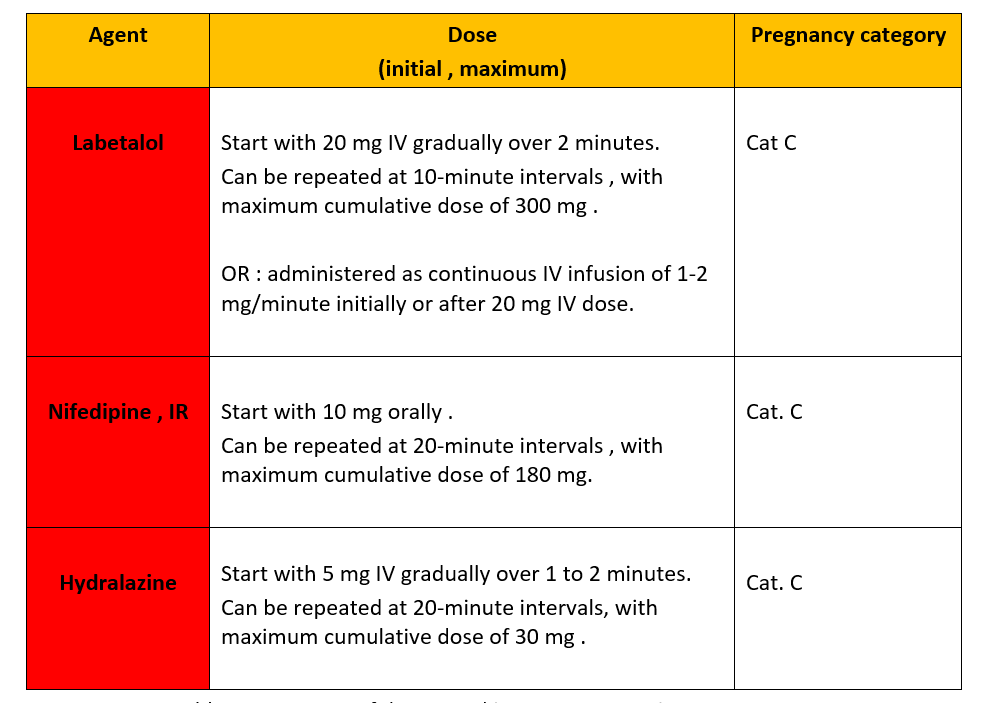
* First-line Drugs used ACUTELY to treat SEVERE blood pressure elevation in pregnancy ( BP ≥160/110 mmHg ) : [2],[11]
1- Labetalol, IV
2- Nifedipine , Immediate release capsules
3- Hydralazine , IV
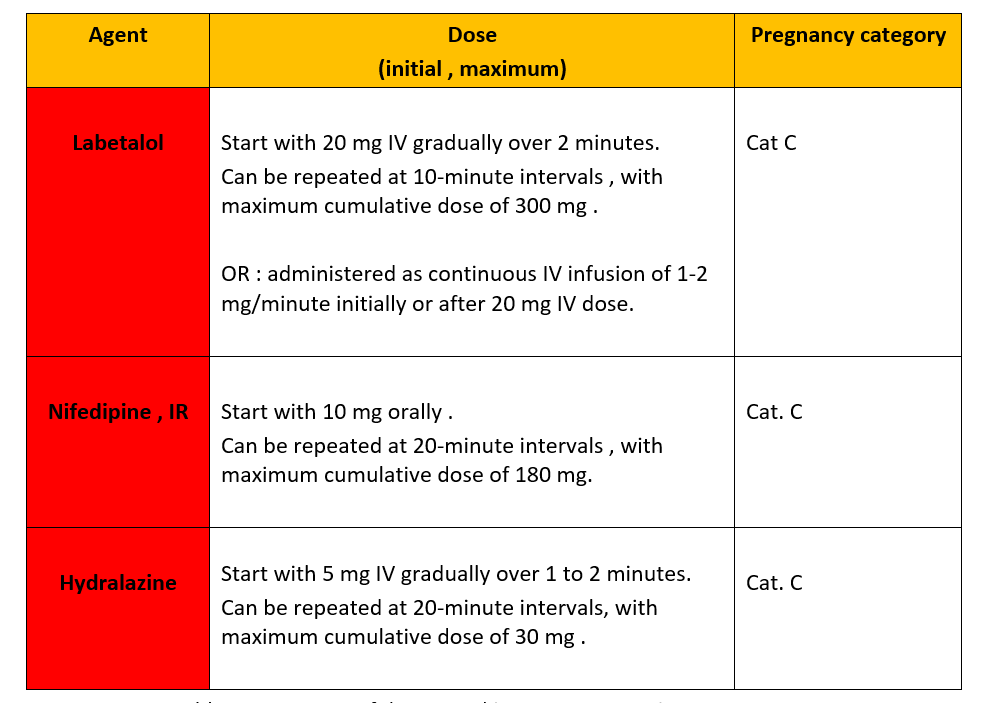
Table 2 : summary of drugs used in SEVERE GHTN in pregnancy
A special thank you to my sister, Rawan Ya’acoub, a clinical pharmacist and assistant professor at the University of Jordan, who helped me write this blog.
References:
[1]- Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020 Jun;135(6):e237-e260. doi: 10.1097/AOG.0000000000003891. PMID: 32443079.
[2]- Diagnosis, Evaluation, and Management of the Hypertensive Disorders of Pregnancy:
Executive Summary . No. 307, May 2014 . Laura A. Magee, MD, Vancouver BC . Anouk Pels, MSc, Amsterdam, the Netherlands . Michael Helewa, MD, Winnipeg MB . Evelyne Rey, MD, Montreal QC . Peter von Dadelszen, MBChB, Vancouver BC.
[3]- Magee LA; CHIPS Study Group, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, Asztalos E, Murphy KE, Menzies J, Sanchez J, Gafni A, Gruslin A, Helewa M, Hutton E, Koren G, Lee SK, Logan AG, Ganzevoort JW, Welch R, Thornton JG, Moutquin JM. Do labetalol and methyldopa have different effects on pregnancy outcome? Analysis of data from the Control of Hypertension In Pregnancy Study (CHIPS) trial. BJOG. 2016 Jun;123(7):1143-51. doi: 10.1111/1471-0528.13569. Epub 2015 Aug 11. PMID: 26265372.
[4]- Bateman BT, Heide-Jørgensen U, Einarsdóttir K, Engeland A, Furu K, Gissler M, Hernandez-Diaz S, Kieler H, Lahesmaa-Korpinen AM, Mogun H, Nørgaard M, Reutfors J, Selmer R, Huybrechts KF, Zoega H. β-Blocker Use in Pregnancy and the Risk for Congenital Malformations: An International Cohort Study. Ann Intern Med. 2018 Nov 20;169(10):665-673. doi: 10.7326/M18-0338. Epub 2018 Oct 16. PMID: 30326014; PMCID: PMC6854680.
[5]- Firoz T, Magee LA, MacDonell K, Payne BA, Gordon R, Vidler M, von Dadelszen P; Community Level Interventions for Pre-eclampsia (CLIP) Working Group. Oral antihypertensive therapy for severe hypertension in pregnancy and postpartum: a systematic review. BJOG. 2014 Sep;121(10):1210-8; discussion 1220. doi: 10.1111/1471-0528.12737. Epub 2014 May 16. PMID: 24832366; PMCID: PMC4282072.
[6]- Mito A, Murashima A, Wada Y, Miyasato-Isoda M, Kamiya CA, Waguri M, Yoshimatsu J, Yakuwa N, Watanabe O, Suzuki T, Arata N, Mikami M, Ito S. Safety of Amlodipine in Early Pregnancy. J Am Heart Assoc. 2019 Aug 6;8(15):e012093. doi: 10.1161/JAHA.119.012093. Epub 2019 Jul 26. PMID: 31345083; PMCID: PMC6761676.
[7]- Magee LA; CHIPS Study Group, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, Asztalos E, Murphy KE, Menzies J, Sanchez J, Gafni A, Gruslin A, Helewa M, Hutton E, Koren G, Lee SK, Logan AG, Ganzevoort JW, Welch R, Thornton JG, Moutquin JM. Do labetalol and methyldopa have different effects on pregnancy outcome? Analysis of data from the Control of Hypertension In Pregnancy Study (CHIPS) trial. BJOG. 2016 Jun;123(7):1143-51. doi: 10.1111/1471-0528.13569. Epub 2015 Aug 11. PMID: 26265372.
[8]- Magee LA, Cham C, Waterman EJ, Ohlsson A, von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003 Oct 25;327(7421):955-60. doi: 10.1136/bmj.327.7421.955. PMID: 14576246; PMCID: PMC259162.
[9]- Cooper WO, Hernandez-Diaz S, Arbogast PG, Dudley JA, Dyer S, Gideon PS, Hall K, Ray WA. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med. 2006 Jun 8;354(23):2443-51. doi: 10.1056/NEJMoa055202. PMID: 16760444.
[10]- Hecker A, Hasan SH, Neumann F. Disturbances in sexual differentiation of rat foetuses following spironolactone treatment. Acta Endocrinol (Copenh). 1980 Dec;95(4):540-5. doi: 10.1530/acta.0.0950540. PMID: 7456979.
[11]- ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019 Feb;133(2):e174-e180. doi: 10.1097/AOG.0000000000003075. PMID: 30575639.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”

 dical wards. He then went on to become the first African-American resident in internal medicine at the University of Maryland School of medicine and the first African-American cardiologist in the state of Maryland in 1965.
dical wards. He then went on to become the first African-American resident in internal medicine at the University of Maryland School of medicine and the first African-American cardiologist in the state of Maryland in 1965.  Despite improvements in health distribution inequalities, African-American communities are continuously plagued with cardiovascular disease at an alarming rate. Some of the main contributors to the high burden of disease are the persistent and increasing degrees of limited access to healthy food, low socioeconomic status, and poor nutritional awareness. To address this, Dr. Saunders advocated for community screening and outreach in barbershops and churches in order to engage the black community in non-traditional spaces. In 2006, he developed the Hair, Heart and Health program, an innovative program that trained barbers and hairstylists to pre-screen customers for hypertension and then make referrals for medical care.
Despite improvements in health distribution inequalities, African-American communities are continuously plagued with cardiovascular disease at an alarming rate. Some of the main contributors to the high burden of disease are the persistent and increasing degrees of limited access to healthy food, low socioeconomic status, and poor nutritional awareness. To address this, Dr. Saunders advocated for community screening and outreach in barbershops and churches in order to engage the black community in non-traditional spaces. In 2006, he developed the Hair, Heart and Health program, an innovative program that trained barbers and hairstylists to pre-screen customers for hypertension and then make referrals for medical care.