Nursing Poster Sessions
Next to the great talks, there are also great posters at the American Heart Association. Some of these posters I would like to highlight in this blog.
Muna Hammash presented that interventions such as psychoeducational before and after ICD insertion may improve perceived control and, in turn, quality of life.
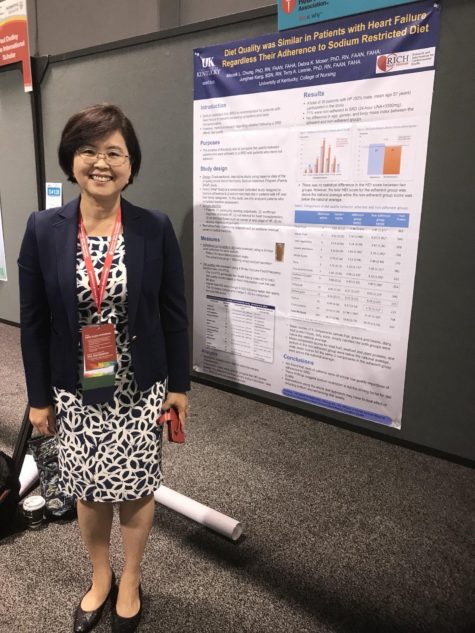
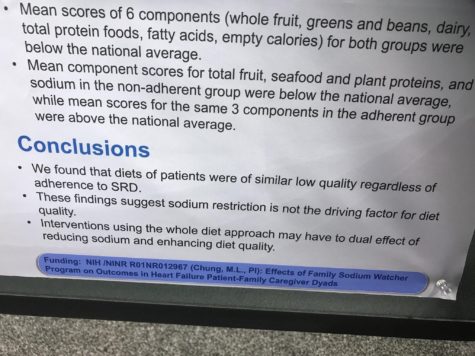
Dr. Misook Chung had an interesting poster on diet quality in patients with heart failure. She found that diet quality was similar in patients with heart failure regardless of their adherence to sodium restriction diet.
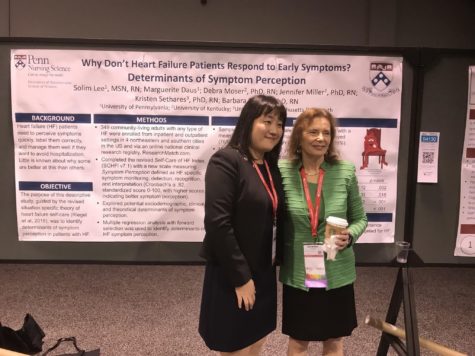
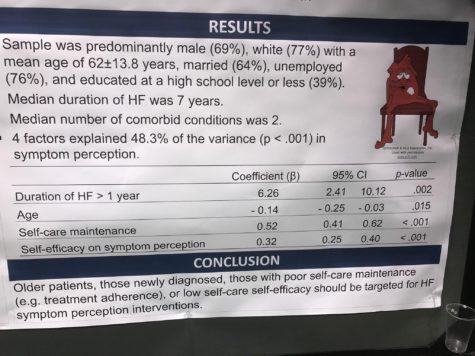
Solim Lee presented why patients with heart failure don’t respond to early symptoms.
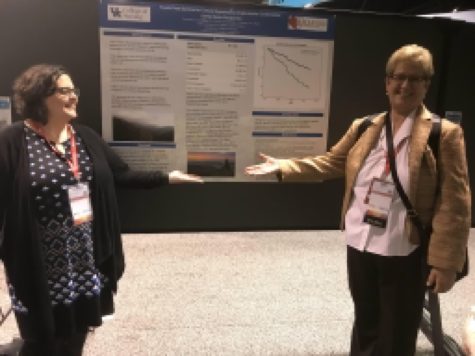
Dr. Jennifer Miller showed that living in a socio economically austere area imparts greater risk for death or hospitalization for ICD recipients.
Hiroko Ishida presented a poster on dyad research. She found that health literacy of patients with heart failure and their caregivers was independently associated with caregivers burden.
Umama Gorsi had an abstract accepted about cardiac rehabilitation. She found that early outpatient cardiac rehabilitation is associated with reduced total mortality rates after myectomy for treatment of hypertrophic cardiomyopathy.
There were great presentation on self-care in patients with heart failure. Foster Osei Baah found in his research that self-care confidence moderates the relationship between marginalization and self-care maintenance in patients with heart failure.
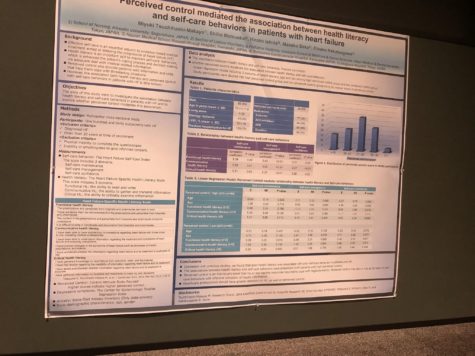
In another research on self-care, Miyuki Tsuchihashi-Makeya found that health literacy was associated with poor self-care. Furthermore, she found that perceived control mediated the association between health literacy and self-care behaviors in patients with heart failure.
I would like to thank all the researchers in this blog for their enthusiasm to discuss their work with me!

Leonie Klompstra is a Nurse Scientist at the Linköping University in Sweden. Her primary focus is on heart failure and rehabilitations.