Anticoagulation In Dialysis Patients: Clear As Mud
End-stage renal disease (ESRD) is a paradox of both increased ischemic and hemorrhagic stroke risk. Atrial fibrillation is prevalent in up to 27% of the ESRD population and further amplifies the stroke risk. However, while the overall ischemic stroke rate is increased 2.5-fold in ESRD as compared to the general population, the rate of hemorrhagic stroke is increased 5-fold due to a complex milieu that includes uremic platelet dysfunction and exaggerated blood pressure fluctuations on hemodialysis.
For over 50 years, warfarin was the only oral anticoagulant available for long-term stroke prevention in atrial fibrillation patients. However, while robust data from randomized controlled trials in the 1980s clearly demonstrated stroke reduction in the general population, we only have observational data in the ESRD population and the evidence here is mixed. Overall, the survival benefit is unclear, and bleeding events are augmented. Warfarin also has the notoriety for increasing the risk of adverse cardiovascular outcomes in the ESRD population. Our group recently published a retrospective analysis of our medical center’s database (spearheaded by medical student extraordinaire Mark Lin) where we noted significantly increased risk of mortality and MI in ESRD patients on warfarin.
Over the past decade we’ve seen the emergence of Direct Oral Anticoagulants (DOACs) that include the direct thrombin inhibitor dabigatran, and the factor Xa inhibitors apixaban, rivaroxaban and edoxaban. Apixaban was approved by the FDA in 2014 for use in ESRD patients, a perplexing move that was based on a single phase 1 study that involved eight hemodialysis patients who were given a single dose of the drug.
At the #AHA17 scientists and colleagues presented trends from the US Renal Data System database that highlights the remarkable spike in apixaban prescriptions for atrial fibrillation among Medicare beneficiaries on chronic dialysis (Nov 12, 2017 Abstract# 17197). About 26,000 patients were included in the final analysis. Utilization of DOACs rose from 0.16% to 29.16% between 2010-2015 with apixaban accounting for the majority of new DOAC prescriptions (see Figure).
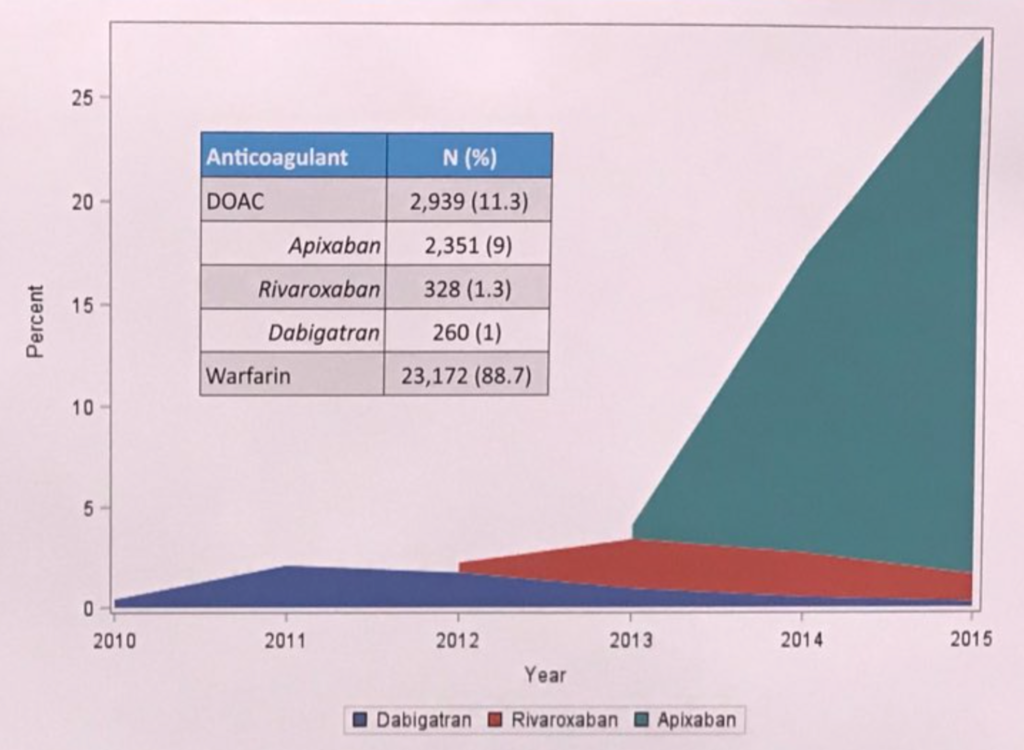 Photo credit @JCosinSales
Photo credit @JCosinSales
Post FDA approval, the observational data has been promising in that apixaban may have lower adverse bleeding rates compared to warfarin. However, a more rigorous pharmacokinetics study published this year in the Journal of the American Society of Nephrology by Mavrakanas et al. raises serious concerns about supratherapeutic blood levels if standard apixaban dosing (5 mg BID) is used in ESRD patients. Until more data is available, the investigators cautioned that apixaban 2.5 mg BID is a more appropriate dosing regimen in dialysis patients.
A randomized clinical trial in ESRD patients with atrial fibrillation is currently ongoing that will directly compare apixaban versus warfarin (RENAL-AF). However, given the lack of a placebo control arm, this trial will not address the fundamental unanswered question: Does anticoagulation, period, decrease stroke risk and improve survival in the ESRD population?
Nephrologists, who manage heparin anticoagulation during hemodialysis treatments and are most attuned to the bleeding risks in ESRD patients, need to be notified when dialysis patients are initiated on anticoagulation. In this complex and high-risk population, ongoing dialogue between the cardiologist, primary care doc and nephrologist is necessary to weigh the risks/benefits of anticoagulation on a case-by-case basis.
Wei Ling Lau MD is Assistant Professor in Nephrology at the University of California-Irvine, where she studies vascular calcification and brain microbleeds in animal models of chronic kidney disease. She is currently funded by an AHA Innovative Research Grant, and has been a speaker for CardioRenal University and the American Society of Nephrology.