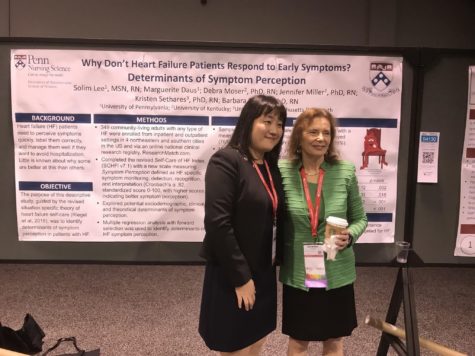
Nursing research at Heart Failure congress 2018 in Vienna, Austria
The 26th-29th of May I went to the Heart Failure Congress 2018, Including the World Congress on Acute Heart Failure in Vienna, Austria. The congress had over 5,750 participants from over 80 countries. To see all the tweets during this congress, search for the #HeartFailure2018.
This year there were a lot of interesting talks and I would like to highlight a few in this blog.
Dr. Tiny Jaarsma gave a talk about sex and heart disease. Pointing out that heart disease can lead to sexual problems. Furthermore, patients think that sexual counseling should be part of cardiac rehabilitation, which is often not a subject that is discussed. Patients prefer to receive written material and/or individual discussions.
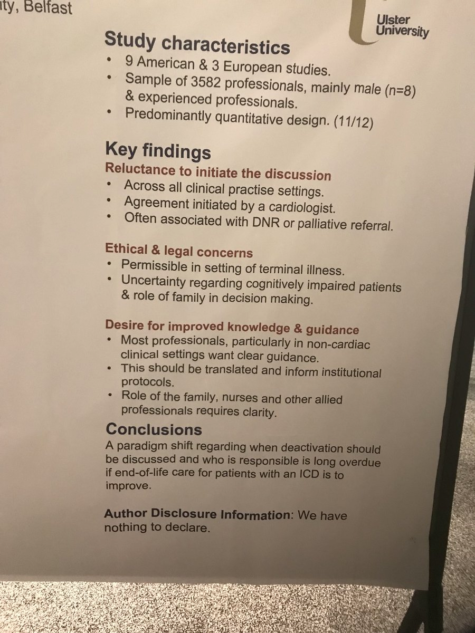
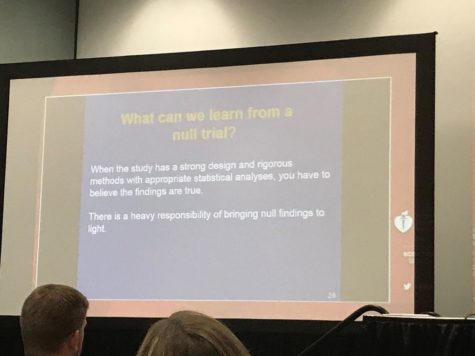
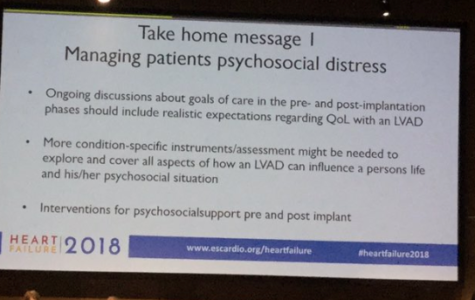
Dr. Cecilia Line from @karolinskaint pointed out that one third of patients with an ICD are not aware that they can deactivate their ICD. Furthermore, patients with ICDs would like to be informed especially when the life expectancy is short. And we should remember, according to Dr. Anna Strömberg, that patients with an LVAD are going through a transition in life and that there are psychosocial challenges in patients with an LVAD. See her take-home messages in the pictures below.
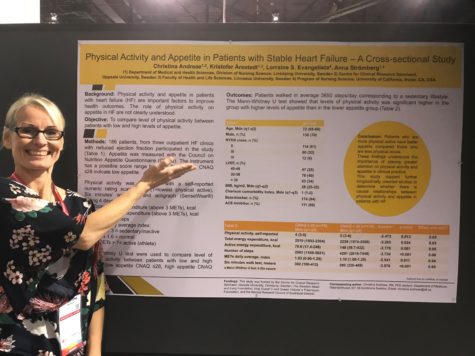
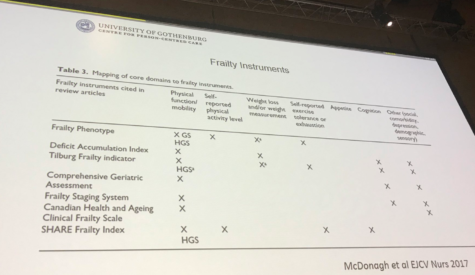
Some talks highlighted the importance of frailty in cardiac patients. Dr. Inger Ekman from @SahlgrenskaAcad discussed the importance of screening for frailty in cardiac patients and suggested existing instruments to do so (see picture below). Dr. Kentaro Kamiya’s research showed that frailty is associated with clinical outcomes in elderly patients hospitalized for heart failure, which indicates that frailty is useful for prognosis in in hospital settings.
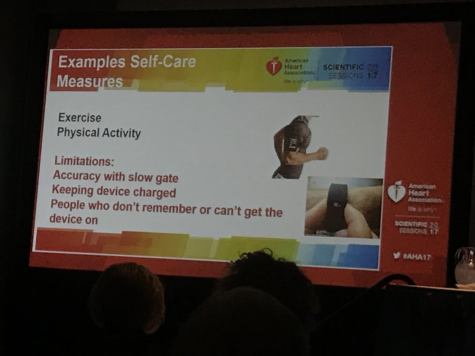
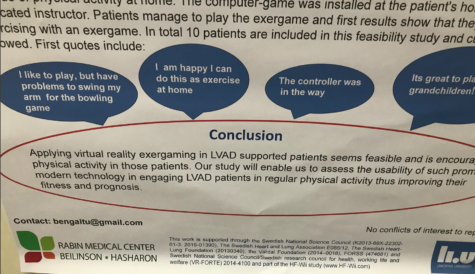
In the late breaking trials, the results of the HF-Wii study were discussed. This study proves that exergaming (being physical active through video gaming) has positive influence with the exercise capacity and wellbeing of patients with heart failure. See an interview about this study during the interview. In a poster presenting a sub-study of the HF-Wii showed that exergaming could also be feasible for patients with an LVAD, and patients especially liked to exergame with their grandchildren.
There was also a great session on alternative ways to be physically active in patients with heart failure. One of the alternative ways was presented by Dr. Anna Strömberg: medi-yoga. Read more about medi-yoga. A second alternative way to exercise was presented by Dr. Taylor-Piliae: Tai-Chi. And a third way presented by Dr. Tiny Jaarsma was exergaming. In this session Dr. Von Haehling pointed out that testosterone therapy could increase exercise capacity. Dr. Massimo Piepoli concluded that half of the patients with heart failure are denied a highly recommended therapy and that scientific societies should strongly promote a well-recognized therapeutic tool to improve exercise capacity, quality of life and outcomes in patients with heart failure.
And last but not least, I would like to congratulate Lilas Ali, who won the nursing investigator award session with her research that showed that person-centered telephone-support is effective in patients with chronic obstructive pulmonary disease and/or chronic heart failure (see picture below).

Please save the date for next years’ Heart Failure congress 2019, 25-28th of May 2019 in Athens, Greece.


Leonie Klompstra is a Nurse Scientist at the Linköping University in Sweden. Her primary focus is on heart failure and rehabilitations.