Cardiovascular Disease in the Filipino American Community: Revisiting Our Beloved Filipino-Comfort Foods
Filipino Americans make up the 3rd largest Asian American group with about 4.2 million living in the United States1. The burden of cardiovascular disease (CVD) in this group is significant, with 1 in 3 having CVD and a 48% increase in Filipina women undergoing coronary bypass surgery or percutaneous intervention (from 3% to 51%)2. Even more ominous, CVD mortality in Filipino Americans is twice as high compared to the general American population (396 per 100,000)2.
You may be wondering what makes Filipino Americans more vulnerable to CVD- the answer is, it’s complicated. The westernization of the Philippines has in large part increased cardiovascular risk factors that continue to affect Filipinos who immigrate to America. The major culprits include unhealthy ultraprocessed foods, fast food options, and the consequences of the stress of “making it” in America while also financially supporting loved ones back home. One study in the New York City area found that Filipino immigrants were more likely to be obese the longer they lived in the US, especially if they lived in the US for >10 years and if they were <30 years old at the time of moving here3.
Here are the following CVD risk factors in Filipino Americans that stand out2:
- Alcohol consumption: 80% of Filipino American men, 50% of Filipina American women
- Smoking: 17% of Filipino Americans
- High Sodium Diet: the average salt intake in the Filipino diet is 12 grams à 8x greater than the American Heart Association’s recommendation of sodium (1.5 g daily)
- Hypertension: >50% of Filipino Americans 50 years and older
- Diabetes: 70% increased risk compared to other Asian Americans
- Obesity: 14% of Filipino Americans (7 out of 10 Filipino adults living in California are obese)
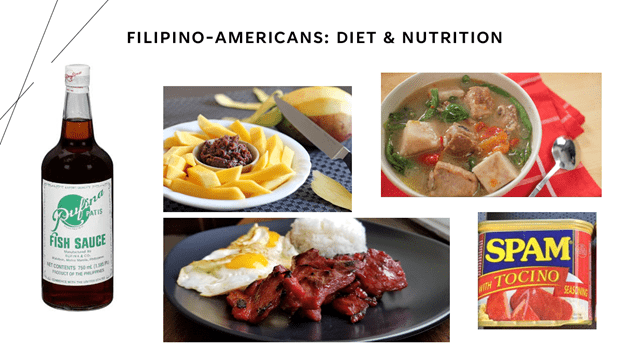
Most, if not all of the above CVD risk factors have one thing in common: the Filipino diet. Before I get crucified for calling out Filipino comfort foods, let me state that as a Filipino-American I very much grew up salivating over Sinigang (tangy tamarind meat or seafood stew) with an extra side of patis (fish sauce), tosilog (sweetly seasoned chicken or pork accompanied by a fried egg and garlic fried rice), and halo-halo (a shaved ice concoction that includes sugar, condensed milk, and other goodies). However, now, as an adult preparing for (hopefully) many decades ahead, it is important to make changes, small or drastic, to improve my chances of having a long and high-quality life with as minimal chronic disease as possible.
Here are my 10 tips and tricks for modifying how we prepare and consume Filipino Foods:
Reduce the amount of salt you cook Filipino dishes with:
- Use low-sodium soy sauce and half the amount in dishes like chicken adobo.
- Skip the patis and bagoong for dishes like sinigang, arroz caldo, tinola, and kare kare and instead add more lemon, calimansi or an alternative non-salt seasoning to satisfy your palette.
- If you are using premade Filipino seasoning mixes, look at the nutrition label for the sodium content and consider using half of the packet or even making your own seasoning from scratch to reduce the amount of salt intake.

Reduce the amount of Filipino carbs:
- Replace your white rice with brown rice, quinoa/brown rice blend, or cauliflower rice to get the added benefits of fiber and the sensation of feeling fuller faster.
- If you crave white rice and cannot live without it, cut your portion in half and fill the rest of the plate with vegetables (garlic green beans, garlic broccoli, sauteed kale/spinach).
- For noodle and pancit lovers, change your ratio of mostly noodles and vegetables/proteins to the complete oppositeà mostly vegetables/lean protein and a quarter portion of noodles
- Our Filipino desserts like halo-halo, mamon, sans rival, ube desserts, leche flan, and bibinka are some of the many indulgences we enjoy. These have a TON of sugar and empty calories but are difficult to modify so instead, only eat these for special occasions 2-3x/year when you are really craving them. Alternative Filipino desserts include fresh fruits like mangoes and whatever fruit is in season. And if you did not know already, Filipino fruit salad is NOT healthy- condensed milk, all-purpose cream, cream cheese, and canned fruit cocktail is FULL OF SUGAR and a one-way road to diabetes.

Reduce the fried and high-fat Filipino foods:
- Love lumpia and ukoy? So do I. If you can afford to use an air fryer select this to save on calories that would come from the oil required to fry these foods. If you do not have an air fryer, consider baking your lumpia.
- For the staple dishes like kare kare, sinigang, nilaga, kaldereta, menudo, and mechado, you have a few options for modifications: 1) select lean meats like chicken or seafood, 2) if you love red meat and cannot live without it then select leaner cuts of red meat and pork, or 3) use your favorite meat but put less amounts in the stew and add more high fiber vegetables
- Stop eating ultraprocessed foods: these include Spam, longganisa, tocino, corned beef, and Vienna sausage. Many of these are canned and have high preservatives, artificial additives, sodium nitrites and nitrates that increase your risk for heart disease, cancer, stroke, and death.
If you’ve reached this paragraph then I will assume you are motivated or at least partially motivated to modify the way you think, prepare, and eat Filipino comfort foods. We can all agree that food culture is incredibly important to living a full and happy life. As a preventive cardiologist, my hope is to help myself, family, friends, and patients strike the balance between enjoying culture while developing healthy habits that will improve our quality of life for the long run.
Stay healthy,
Dr. Kyla Lara-Breitinger
References:
- Pew Research: Over 4.2M Filipino Americans in the US — (asianjournal.com)
- Sales et al. Philippine and Philippine-American Health Statistics, 1994-1018. CARE Data Brief Feb 2020.
- Afable A et al. Fam Community Health. 2016 Jan-Mar;39(1):13-23.
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”

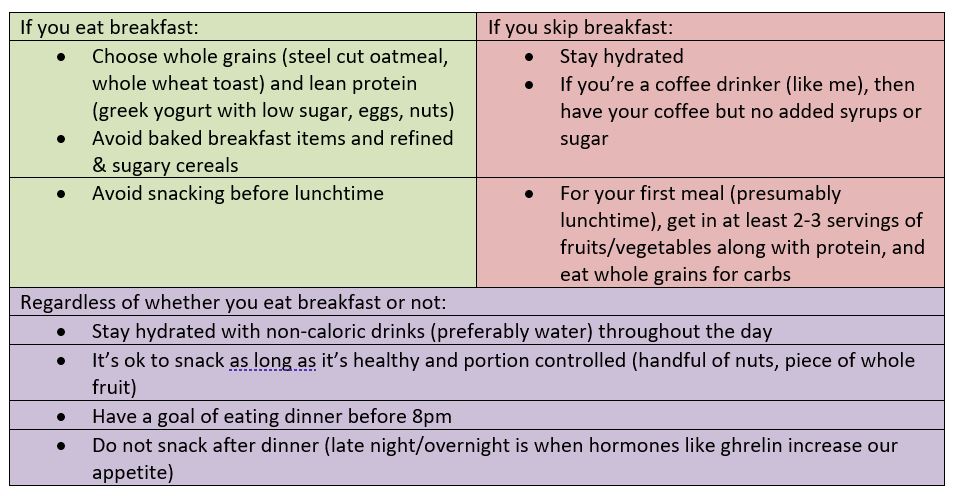



 Unsurprisingly, almost all of my patients I’ve seen over the past year have fallen victim to this, with good reason. They are protecting their health by avoiding exposure to COVID-19 but at the same time are unconsciously neglecting their health by not having the means or green light to engage in healthy behaviors such as going to the gym, walking in public spaces, and engaging in aerobic exercise and strength training. Our current restrictive environment combined with more time at home to eat and indulge is a fail-proof setup for adding on these harmful extra pounds.
Unsurprisingly, almost all of my patients I’ve seen over the past year have fallen victim to this, with good reason. They are protecting their health by avoiding exposure to COVID-19 but at the same time are unconsciously neglecting their health by not having the means or green light to engage in healthy behaviors such as going to the gym, walking in public spaces, and engaging in aerobic exercise and strength training. Our current restrictive environment combined with more time at home to eat and indulge is a fail-proof setup for adding on these harmful extra pounds. For many of us, we understand what we should eat to become healthier, however, that does not mean we will actually follow this rationale to maintain a heart-healthy diet, especially during a pandemic when most of our day is spent sedentary in isolation at home. Despite having a master’s degree in Nutrition as part of my training, I can admit that I have invariably fell victim to the vices of food comfort at home. I was eating a lot of baked desserts after dinner but recently decided to replace this habit with a cup of hot chocolate made with soy milk and sugarless cocoa powder.
For many of us, we understand what we should eat to become healthier, however, that does not mean we will actually follow this rationale to maintain a heart-healthy diet, especially during a pandemic when most of our day is spent sedentary in isolation at home. Despite having a master’s degree in Nutrition as part of my training, I can admit that I have invariably fell victim to the vices of food comfort at home. I was eating a lot of baked desserts after dinner but recently decided to replace this habit with a cup of hot chocolate made with soy milk and sugarless cocoa powder. When news of the approval of the Pfizer vaccine surfaced, I felt a sense of anxiety. There was no data on pregnant women in the COVID-19 vaccine trials. As a medical professional, we have been trained to apply for evidenced-based medicine and baseline patient characteristics of trial participants to the patients we plan to treat. But what if your pregnancy status was not studied in the trial during a global pandemic? How might you weigh the unknown risks of the vaccine to your growing fetus with the risk of COVID-19 infection while pregnant?
When news of the approval of the Pfizer vaccine surfaced, I felt a sense of anxiety. There was no data on pregnant women in the COVID-19 vaccine trials. As a medical professional, we have been trained to apply for evidenced-based medicine and baseline patient characteristics of trial participants to the patients we plan to treat. But what if your pregnancy status was not studied in the trial during a global pandemic? How might you weigh the unknown risks of the vaccine to your growing fetus with the risk of COVID-19 infection while pregnant?