Environmental and Neighborhood Influences on Health at #AHA19
Where we live and work shapes us in many ways. Whether growing up in an urban, suburban, or rural community, our neighborhoods can have an outsized impact our hobbies, lifestyle, and health. It was inspiring to see so many investigators presenting findings on this topic today at the American Heart Association (AHA) 2019 Scientific Sessions during the “Environmental and Neighborhood Influences on Health” poster session.
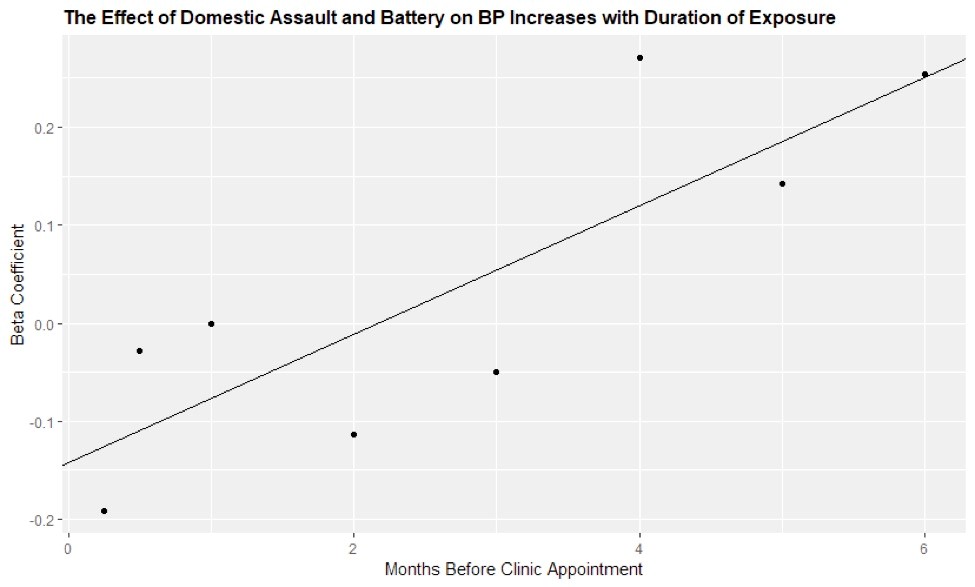
W. Wyatt Wilson and colleagues at the University of Chicago presented “Spatiotemporal Association Between Violent Crime And Ambulatory Elevations In Systolic Blood Pressure”, an innovative analysis of 133,024 geo-coded violent crimes reported by the City of Chicago and home addresses of patients with blood pressure readings from 232,488 unique outpatient appointments. They found that longer duration of exposure to violent crime within 500 meters of patients’ home addresses was associated with increased systolic blood pressure (approximately 0.27 mmHg per crime) [Figure 1]1. These results echo findings from the Jackson Heart Study published earlier this year by Tanya M. Spruill and colleagues on chronic stress and incident hypertension among black adults2. This analysis followed 1,829 adults without hypertension over a median of 7 years and recorded their blood pressure and self-reported stress. After multi-variable adjustment, they found moderate or high perceived stress was associated with higher risk of developing hypertension. The chronic health effects of stress resulting from living in a neighborhood with violent crime is a newly identified and very significant externality of these crimes.
Figure 1:
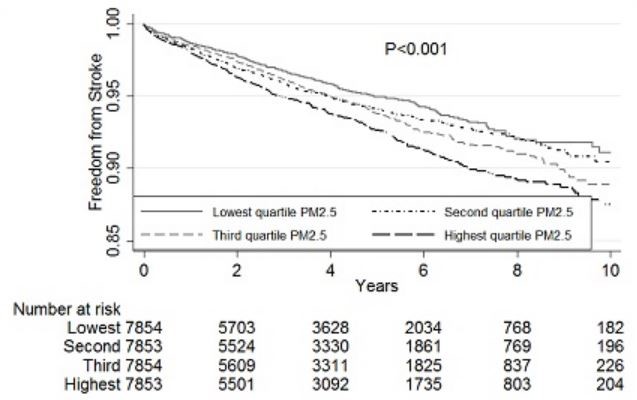
Daniel W. Riggs and colleagues at the University of Louisville presented findings on the interaction between neighborhood greenness, air pollution, and arterial stiffness3. This cross-sectional study of 63 adults measured: neighborhood greenness (satellite-derived normalized difference vegetation [NDVI] index), air pollution (particulate matter [PM] 2.5 levels and ozone levels), and arterial stiffness (augmentation pressure, pulse pressure, and aortic systolic pressure in mmHg). They found among participants living in low greenness areas that air pollution was positively correlated with arterial stiffness. Further, Zachary Rhinehart and colleagues at the University of Pittsburgh presented their poster “Association of Particulate Matter and Incident Stroke in Atrial Fibrillation” which was a retrospective study of 31,414 patients at their academic medical center4. They found that among patients diagnosed with atrial fibrillation, living in neighborhoods with high levels of air pollution (highest quartile compared to lowest quartile) was associated with an increased risk of stroke (HR 1.50; CI 1.30 – 1.72) [Figure 2]. Given such consistent findings between air pollution and cardiovascular disease, I wonder if built environment interventions such as increased vegetation might help mediate neighborhood factors that contribute to cardiovascular disease long-term.
Figure 2:
Attending scientific sessions this year was a phenomenal experience. I came away with new insights for clinic from the late breaking trial sessions, met some incredibly smart and gifted people, and as evidenced by this specific session came away with a renewed enthusiasm to research some questions I was left with. Looking forward to #AHA20!
References:
- W. Wilson et. al. Spatiotemporal Association Between Violent Crime And Ambulatory Elevations In Systolic Blood Pressure. Poster Presentation, American Heart Association 2019 Scientific Sessions, Philadelphia, PA, November 18, 2019 https://www.ahajournals.org/doi/10.1161/circ.140.suppl_1.17139
- J Am Heart Assoc. 2019;8:e012139. DOI: 10.1161/JAHA.119.012139.
- W. Riggs et. al. Effect Modification of Neighborhood Greenness on the Relationship Between Ambient Air Pollution and Arterial Stiffness. Poster Presentation, American Heart Association 2019 Scientific Sessions, Philadelphia, PA, November 18, 2019 https://www.ahajournals.org/doi/10.1161/circ.140.suppl_1.15881
- Rhinehart et. al. Association of Particulate Matter and Incident Stroke in Atrial Fibrillation. Poster Presentation, American Heart Association 2019 Scientific Sessions, Philadelphia, PA, November 18, 2019 https://www.ahajournals.org/doi/10.1161/circ.140.suppl_1.16440
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.

 I have gone back and forth with attending the American Heart Association (AHA) Scientific Sessions online in 2017 (AHA17), to onsite (AHA18), and this year (AHA19) I attended online again. There was absolutely no comparison between attending AHA18 to the online versions! I was the first to say that going to conference is overwhelming because there is so much to see and so many people to meet. I have since come to appreciate the benefits to attending meetings onsite. Generally, I stay within my session [Atherosclerosis, Thrombosis, Vascular Biology (ATVB) or Hypertension (HTN)]. Attending online gives some limitations, such as being at home, work, or traveling, there is a time restraint as well as multiple distractions. I experienced them all! I was traveling to a conference that conflicted with AHA19, thus the distractions of traveling and keeping up with my meeting responsibilities was a lot to juggle. Once I was home, there was everything that goes along with getting settled back into the routine of things that gave me a distraction. This year was a beast of responsibilities, but before I discourage you from attending a meeting online, let me share some benefits and things that I enjoyed about having the flexibility of being online rather than onsite.
I have gone back and forth with attending the American Heart Association (AHA) Scientific Sessions online in 2017 (AHA17), to onsite (AHA18), and this year (AHA19) I attended online again. There was absolutely no comparison between attending AHA18 to the online versions! I was the first to say that going to conference is overwhelming because there is so much to see and so many people to meet. I have since come to appreciate the benefits to attending meetings onsite. Generally, I stay within my session [Atherosclerosis, Thrombosis, Vascular Biology (ATVB) or Hypertension (HTN)]. Attending online gives some limitations, such as being at home, work, or traveling, there is a time restraint as well as multiple distractions. I experienced them all! I was traveling to a conference that conflicted with AHA19, thus the distractions of traveling and keeping up with my meeting responsibilities was a lot to juggle. Once I was home, there was everything that goes along with getting settled back into the routine of things that gave me a distraction. This year was a beast of responsibilities, but before I discourage you from attending a meeting online, let me share some benefits and things that I enjoyed about having the flexibility of being online rather than onsite.