Housing and Health Equity in Cardiovascular Disease
So far, 2020 has been a year of public health crises. By early spring, it was apparent that people living in socio-economically disadvantaged areas were being hit hardest by Covid-19 [1]. In these same areas, people across the United States took to the streets protesting the murder of George Floyd, an unarmed Black man – in police custody [2]. In the words of James Baldwin, “It demands great spiritual resilience not to hate the hater whose foot is on your neck, and an even greater miracle of perception and charity not to teach your child to hate.”, and we as a country are still looking for this resilience [3]. Among the many consequences of this year’s events, these tragedies have really prompted a long, hard look at our healthcare system. One recently published article that was particularly heartening to read was the American Heart Association’s Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research Scientific Statement on “Importance of Housing and Cardiovascular Health and Well-Being”. It outlines how housing stability, quality, affordability, and neighborhood environment are linked to cardiovascular disease. The statement doesn’t shy away from evidence of how increased psychosocial stress in the Black community and other social determinants of health are associated with cardiovascular health disparities.
The world has changed profoundly over the past year and while we continue to strive to show charity to others in our everyday encounters, I look forward to reading more research that will help inform how we as a community can better address health inequity.
References:
- Chowkwanyun M, Reed AL Jr. Racial Health Disparities and Covid-19 – Caution and Context. N Engl J Med. 2020;383(3):201-203. doi:10.1056/NEJMp2012910 (https://www.nejm.org/doi/full/10.1056/NEJMp2012910)
- Taylor, Derrick Bryson. “George Floyd Protests: A Timeline.” The New York Times, The New York Times, 30 May 2020, www.nytimes.com/article/george-floyd-protests-timeline.html. (https://www.nytimes.com/article/george-floyd-protests-timeline.html)
- Baldwin, James, 1924-1987. The Fire next Time. New York: Dial Press, 1963. (https://www.newyorker.com/magazine/1962/11/17/letter-from-a-region-in-my-mind)
- Sims M, Kershaw KN, Breathett K, Jackson EA, Lewis LM, Mujahid MS, Suglia SF; on behalf of the American Heart Association Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research. Importance of housing and cardiovascular health and well-being: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2020;13:e000089. doi: 10.1161/HCQ.0000000000000089 (https://www.ahajournals.org/doi/10.1161/HCQ.0000000000000089)
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”
 [4]
[4]

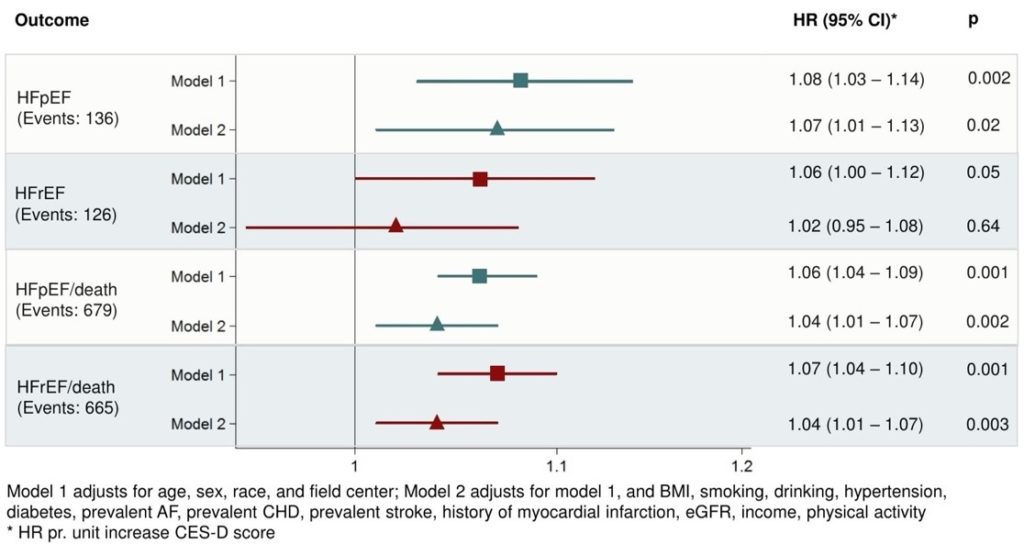
 Two other groups of researchers presented similar findings with depression and heart failure. An analysis of The Atherosclerosis Risk in Communities Study (ARIC) presented by Katja Vu from Brigham and Women’s Hospital found a relationship between depression and incidence of heart failure with preserved ejection fraction (HR 1.07; CI 1.02 – 1.13) among older adults (mean age 75 years) of both sexes3. However, there was no such relationship with incidence of heart failure with reduced ejection fraction [Figure 1]. Yosef Khan from the American Heart Association presented National Health and Nutritional Examination Survey (NHANES) data suggesting that depression increases risk of heart failure, coronary disease, or cerebrovascular disease even after adjusting for Life’s Simple 7: physical exercise, heart healthy diet, weight, blood pressure, cholesterol, blood sugar, and tobacco use4.
Two other groups of researchers presented similar findings with depression and heart failure. An analysis of The Atherosclerosis Risk in Communities Study (ARIC) presented by Katja Vu from Brigham and Women’s Hospital found a relationship between depression and incidence of heart failure with preserved ejection fraction (HR 1.07; CI 1.02 – 1.13) among older adults (mean age 75 years) of both sexes3. However, there was no such relationship with incidence of heart failure with reduced ejection fraction [Figure 1]. Yosef Khan from the American Heart Association presented National Health and Nutritional Examination Survey (NHANES) data suggesting that depression increases risk of heart failure, coronary disease, or cerebrovascular disease even after adjusting for Life’s Simple 7: physical exercise, heart healthy diet, weight, blood pressure, cholesterol, blood sugar, and tobacco use4.