The DAPA-HF trial was definitely the highlight of the scientific sessions at the AHA19 conference. I’m fascinated by the interesting outcomes and keen to learn more about the effect of SGLT-2 inhibitors on heart failure (HF) patients with preserved ejection fraction (HFpEF). In the next few lines, I’m going to briefly discuss the significant findings of DAPA-HF that were presented at AHA19, and will sooner nor later change the guidelines for management of patients with HFrEF.
Sodium-glucose cotransporter-2 inhibitor (SGLT-2 inhibitor) are relatively new class of drugs that act on inhibiting glucose reabsorption from proximal tubules, and thus decrease serum blood glucose concentrations.1 They are commonly prescribed to treat T2DM patients who have poor glycemic control. However, new data are emerging in large support of the beneficial effects of SGLT-2 inhibitors not just on diabetics but also on non-diabetic HF patients. The data is big and clear as presented by Dr. John McMurray at AHA19 and it is expected to list SGLT-2 inhibitors such as dapagliflozin (Farxiga) as guideline directed medical therapeutics (GDMT) in 2021 for HF patients.
In the DAPA-HF, McMurray and colleagues enrolled 4,744 patients with heart failure characterized by reduced ejection fraction (defined as left ventricle ejection fraction of 40% or less) from 20 different countries. There were 2,139 patients diagnosed with diabetes who were more likely to have HF etiology of ischemia when compared to non-diabetic patients with HF. The study population consisted of high risk middle aged patients with a mean LV ejection fraction of 31%. The primary end point was a composite outcome consisted of cardiovascular death, HF hospitalization and urgent HF hospital visits over an average of 18 months. As for diabetics in the DAPA-HF trial there was a 25% reduction of CV events (HR 0.75, 95% CI 0.63-0.90) when comparing dapagliflozin against placebo. While, there was a 27% reduction among those who did not have diabetes (HR 0.73, 95% CI 0.59-0.91).2
“The relative and absolute risk reduction in death and hospitalization were substantial, clinically important and consistent across the age spectrum and baseline health status in both patients with or without diabetes”, McMurray noted.
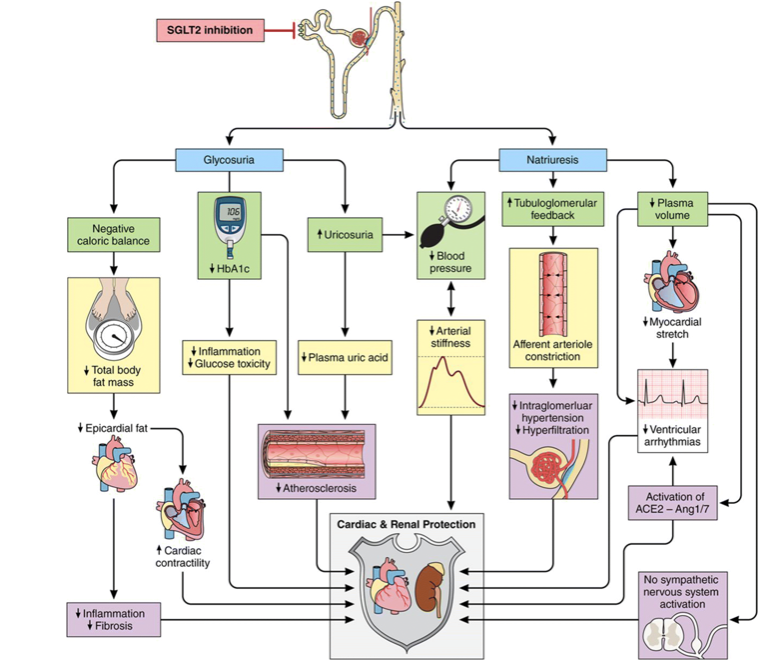
The mechanism by which dapagliflozin provides the cardiovascular benefits that has been documented in the DAPA- HF trial remains to be unclear. It is plausible that SGLT-2 inhibition modifies many CV risk factors such as BP, visceral adiposity, arterial stiffness, hyperinsulinemia, albuminuria, circulating uric acid levels and oxidative stress. These factors are involved in several pathways related to the cardiorenal outcome, where SGLT-2 inhibitors regulate the glucose and sodium excretion and therefore modify the factors in these pathways.
Below is an illustration that explains the proposed pathways involved in cardioprotective role of SGLT-2 inhibitors3
In conclusion, dapagliflozin offers new approaches to the treatment of HF with reduced ejection fraction (HFrEF) in patients with or without diabetes. Data from the DAPA-HF trail provides robust support for the initiation of SGLT-2 inhibitors in patients who either have an established CVD or at risk of developing CVD, and HF in particular, or at risk for renal decline and progression into chronic kidney disease (CKD).
References:
- Mcmurray, John J. V., Demets, David L., Inzucchi, Silvio E., et al. A trial to evaluate the effect of the sodium–glucose co‐transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA‐HF. European Journal of Heart Failure. 2019;21(5):665-675. doi:10.1002/ejhf.1432
- Packer, Milton. Lessons learned from the DAPA-HF trial concerning the mechanisms of benefit of SGLT2 inhibitors on heart failure events in the context of other large-scale trials nearing completion. Cardiovascular diabetology. 2019;18(1):129. doi:10.1186/s12933-019-0938-6
- Ali, Amar, Bain, Steve, Hicks, Debbie, et al. SGLT2 Inhibitors: Cardiovascular Benefits Beyond HbA1c-Translating Evidence into Practice. Diabetes therapy : research, treatment and education of diabetes and related disorders. 2019;10(5):1595-1622. doi:10.1007/s13300-019-0657-8
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.