How to Ensure Accurate Public Communication and Information Sharing
Public communication and knowledge dissemination are often thought of as straight cut, on/off types of action, especially in medicine and the broader health sciences. However it is also very evident in our present day that miscommunication and inaccurate knowledge sharing exists, and has increasingly harmful consequences on the global population. Examples of this are plenty, such as the anti-vaccination movement, the numerous debates about food health categorization, novel diet constructions, and many others.
This year in Philadelphia, where the annual AHA meeting (#AHA19) was hosted, many relevant hot topics in medicine and healthcare were spotlighted, as is usually the case in these types of marquee events. The sense coming out of the meeting was that two major issues of discussion will have to be reckoned with:
- The strong AHA call to action against the E-cigarette proliferating market, specifically in the way it targets youth and minority groups;
- The global trial called ISCHEMIA (International Study of Comparative Health Effectiveness With Medical and Invasive Approaches), with its top-line statement that there was no difference between interventionist and conservative therapies for patients diagnosed with stable ischemic heart disease.
Debates quickly flared, and the messages became misunderstood and controversial. These provide a real life test once again, on how we must optimize public communication and knowledge dissemination.
At #AHA19, the start of the #QuitLying campaign against the forces driving the steep increase in youth consumption of nicotine-containing vaping products, has garnered welcome applause and support by numerous school boards, concerned parents, and health conscious youths, former users of e-cigarettes or not. These groups are well aware of the high prevalence of use (more than 1 in 4 adolescents self report1 as e-cigarette users within the past 30 days, in 2019). Everyone is genuinely concerned about the ramifications if nothing is done. This is why the AHA has stepped up with the #QuitLying initiative to combat against the big industry players that drive the majority of the proliferation of these products within youth culture.
However when the message and information being distributed is counteracted by other sources that aim to mislead and obscure facts, public communication and knowledge sharing becomes much more convoluted and disrupted. Everyone has the right to voice their opinion, that’s not in question, and there is no way to avoid lies and deceptive facts from being shared. But there are new tools to clarify, and focus-deliver facts and evidence-based information to the public that deserves the highest quality data and analysis available to it.
The ISCHEMIA trial debate is another #AHA19 event that requires some clarification and focused-delivery of facts to the public. Some specific details of the trial are nicely outlined by my colleagues Dr. Renee Bullock-Palmer2 and Dr. Adham Karim3, and the primary medical publications from the NIH database are available4 for review by whomever is interested in the full datasets from the sources. The issues I’m addressing here are not with the trial itself, but the resulting real world consequences that form after the debate from ISCHEMIA gets filtered thru multiple gateways, many well-meaning reporters, and some opinion dispensers that lean one way or another regarding the results of the trial.
When public communication and knowledge dissemination is unidirectional and gated, patients can become misinformed and fueled with distrust towards the working relationships they have with their healthcare providers (doctors, nurses, surgeons, medical professionals and hospitals). This can lead to compromised decision making, and potentially harmful health outcomes. Optimizing communication and focused-delivery of evidence-based information are essential goals in our present day world, especially between the medical research and healthcare field, and the general public being served.
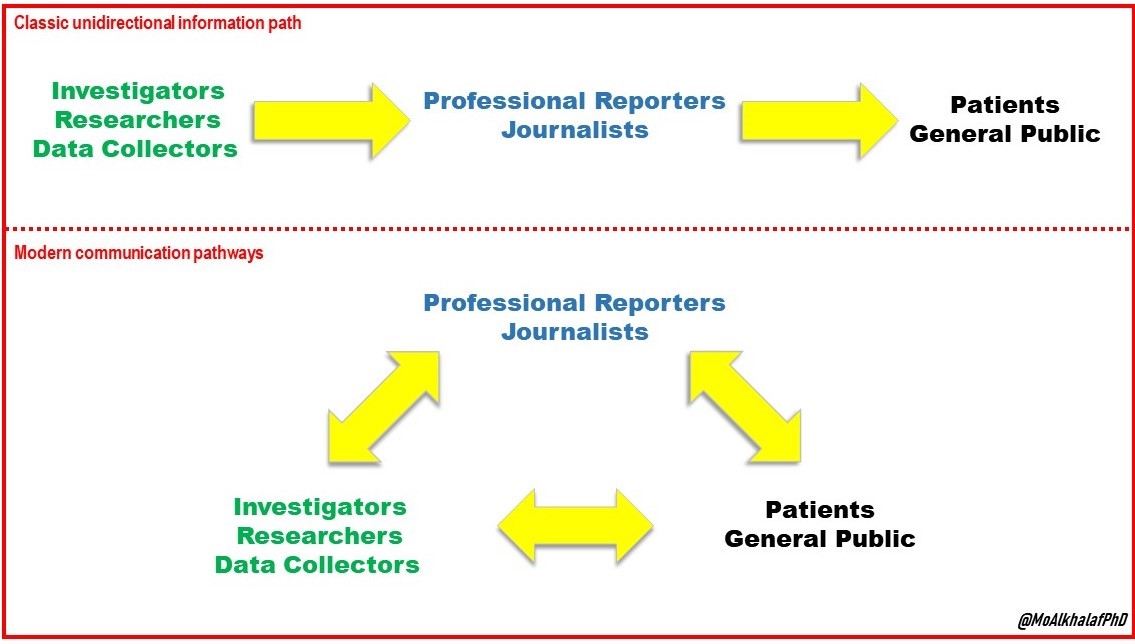
For many decades, from the initial beginnings of professional journalism and news reporting, up to the start of the new millennium, the available and universally accepted method of public communication and knowledge dissemination was a unidirectional pathway: researchers that perform primary data generation and analysis → reporting and communication by well established, reliable and accountable organizations → the public learning of new information that relates to their health and well-being. That being said, presently communication methods are not confined to the same gated, unidirectional path necessarily. The value of professionals in news reporting and communication is still high, and their existence is an asset and a necessity, especially in situations where communication has to be as widespread as possible in as short a time as is necessary. However, we need to encourage, promote, and build pathways that facilitate communication between the primary sources of data, and the general public, so that accuracy and integrity of the information is maintained, and trust is strengthened between all.
Everyone gains when public communication and knowledge dissemination is accurately spread, and trust is established and elevated when stakeholders are not walled off, so that they can be reachable and communicated with. Social media platforms, professional avenues to connect researchers to the public (like this one! The Early Career Voice) are pathways that can and should be used and widely encouraged, mainly as an effort to create a new model of communication that will reduce inaccuracy of information, increase the sense of trust between the public and those who serve it, and help us all lead a healthier life.
References:
- Miech, Richard, et al. “Trends in adolescent vaping, 2017–2019.” New England Journal of Medicine15 (2019): 1490-1491.
- Bullock-Palmer, Renee, MD, “My Top 10 Take Home Points from The ISCHEMIA Trial”, The Early Career Voice, November 18, 2019; (Page Link Here)
- Karim, Adham, MD, “A Few Things the Critical Care Cardiologist Might Have Missed While Talking About the #ISCHEMIA Trial”, The Early Career Voice, November 18, 2019; (Page Link Here)
- ClinicalTrials identifier: NCT01471522; NIH U.S. National Library of Medicine; (Link)
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.
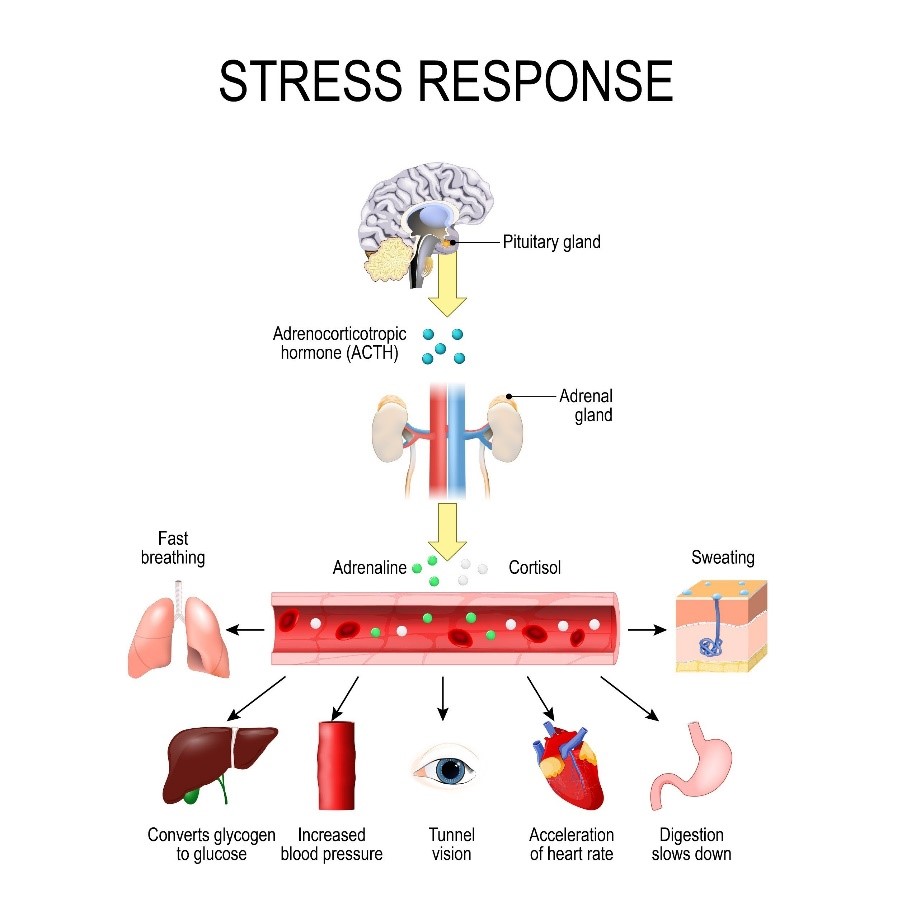 Research continues to mount showing that stress affects our health and well-being. The various daily experiences we face that lead to stress set off a cascade of physiological responses that, when experienced over a lifetime, can lead to diabetes, hypertension, and eventually heart attack and stroke.
Research continues to mount showing that stress affects our health and well-being. The various daily experiences we face that lead to stress set off a cascade of physiological responses that, when experienced over a lifetime, can lead to diabetes, hypertension, and eventually heart attack and stroke.