“Run, Forrest, Run!” – Effects of Cardiovascular Exercising on Mental Health

Source:pixabay
If life gave me a box of chocolates, I am pretty sure I would eat them all. As a basic science researcher, I am all too familiar with burn-outs and stress, and more recently to the effects of stress-induced anxiety. So, I started running. I ran when my worries got too overwhelming, I ran when I had a bad day in the lab. Next thing I knew, I was running for pleasure. And this is something I did not see coming, especially because I hated running before!
Long before medications were available or even prescribed for mental or emotional disorders, exercising remained the only prescription for tacking problems of mental health by doctors.1 The AHA recommends 150 minutes of moderate-high intensity aerobic exercising a week for adults. Researchers have found this to improve balance of neurotransmitters and show effects as early as the first thirty minutes.
Here are some evidence-based effects of exercising on mental health –
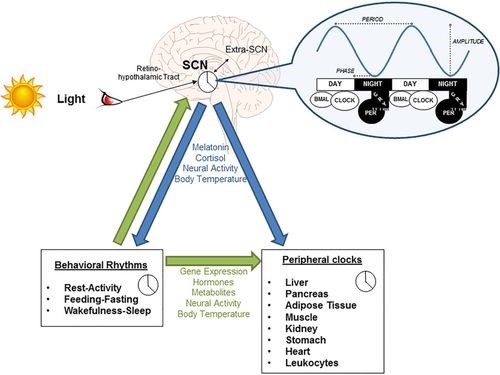
- Stress and anxiety – Chronic stress can shrivel parts of the brain. Exercises have found to reverse this effect and even induce growth of neurons and improve synaptic plasticity in the brain.1,2
- Depression – Regular aerobic exercising can improve blood circulation to the brain and it is known to positively influence hypothalamus-pituitary-adrenal axis of the brain. All of this bounce back the balance of neurotransmitters, elevate mood, attenuate stress and fight back fear.3
- Addiction – While dealing with addiction, exercising has been shown to give a sense of control. Individuals with a tendency to be obsessive, need to fill a void quickly and exercising has shown to be effective in this regard.
- Hormonal fluctuations in women – Hormones estrogen and progesterone play an important role for neurotransmitter in the brain, by providing receptors for them to bind. In some women, this complex pathway can behave in a way that increases aggressive behavior which is found to be dramatically reduced by exercise. Exercising is certainly known to increase levels of tryptophan, the precursor to the happy chemical serotonin. This helps in dealing with the constant fluctuations of hormones during a cycle.1
- Attention deficits – Aerobic exercising has been successful with disorders of distractions, improving focus, concentration and memory of a task.
As with any given task, starting it – is always a challenge. If you are someone like me who is a novice at running, or the thought of running itself induces fear and anxiety – then start with small steps. Take a walk, slowly increase that to brisk walking and when you feel comfortable start jogging. It doesn’t necessarily even need to be running – jumping rope, biking, throwing ball – any activity that spikes your heart rate are good.
So, will you run away from your problems?
References:
- John Ratey, Spark: The Revolutionary New Science of Exercise and the Brain, ISBN:0316028355
- Carek PJ, Laibstain SE, Carek SM, Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41(1):15-28.
- Toups M, Carmody T, Greer T, Rethorst C, Grannemann B, and Trivedi MH. Exercise is an effective treatment for positive valence symptoms in major depression. J Affect Disord 2017; 209: pp. 188-194