Atherosclerosis and Osteoarthritis: Understanding the Impact of being Physical Active
Nearly everyone can experience health benefits from being physically active. Simply, brisk walking can be “go to” for a safe and effective tool to improve or maintain current activity levels.
Physical activity continues to be encouraged because of the staggering impact it has on delaying death from all causes (i.e. heart disease).
The Physical Activity Guidelines for Americans report people who are physically active for approximately 150 minutes a week to have a 33 percent lower risk of all-cause mortality. More importantly, these 150 minutes can be spread throughout a 24 hour period. The benefits accumulate (CDC, 2021).
Thus, avoiding a sedentary lifestyle or even prolonged periods of sitting will maintain a healthy vascular system and keep the heart pumping the way you need it. There is evidence showing that as little as 10 minutes of sitting results in changes that impact microcirculation of blood (Vranish et al., 2018). This microcirculation area is the final destination of the cardiovascular system, and ultimately where oxygen is exchanged.
Breaking up the day into brief bouts of activity goes a long way. So those reminders on the fitness trackers, make sure to use them to your advantage. If you have some health goals you want to meet, use physical activity tracking as a supplement to your plan. Walking an additional 1000 steps per day can help lower the risk of all-cause mortality, and cardiovascular disease morbidity and mortality in adults (Hall et al., 2020).
A study published by Wolf et. al. showed that even four-second bouts of intense activity between bouts of sitting can carry benefits that extend into the next day. In a model of 8 hours of inactivity, study participants cycled five times every hour over a 6 hour period. These exercise bouts from the previous day reduced levels of fat in the blood by 31% (Wolfe et al., 2020).
However, not everyone can just get up and move. Individuals that are diagnosed with osteoarthritis of the hip and knee represent one of the leading causes of global disability (Skou et al., 2018). Thus, a group like this will struggle to meet activity guidelines and is likely to share an increased burden of cardiovascular disease risk. The presence of osteoarthritis in a large prospective cohort (1,775) followed over a mean of 8 years showed an increased risk of cardiovascular disease by 27% (Veronese et al., 2018). Determining ways to encourage physical activity even in disabling scenarios/conditions, continues to be a challenge. Magnetic resonance (MR) imaging, one of the most advanced imaging techniques used clinically, could be used to inform physicians how to best to approach this challenge. In a brief review by Liu et. al., MR images were used to visualize lower limbs to aid in the development of biomarker development and/or predict patients with risk to PAD. This could patients who are inactive because of the severity of osteoarthritis (Liu et al., 2019).
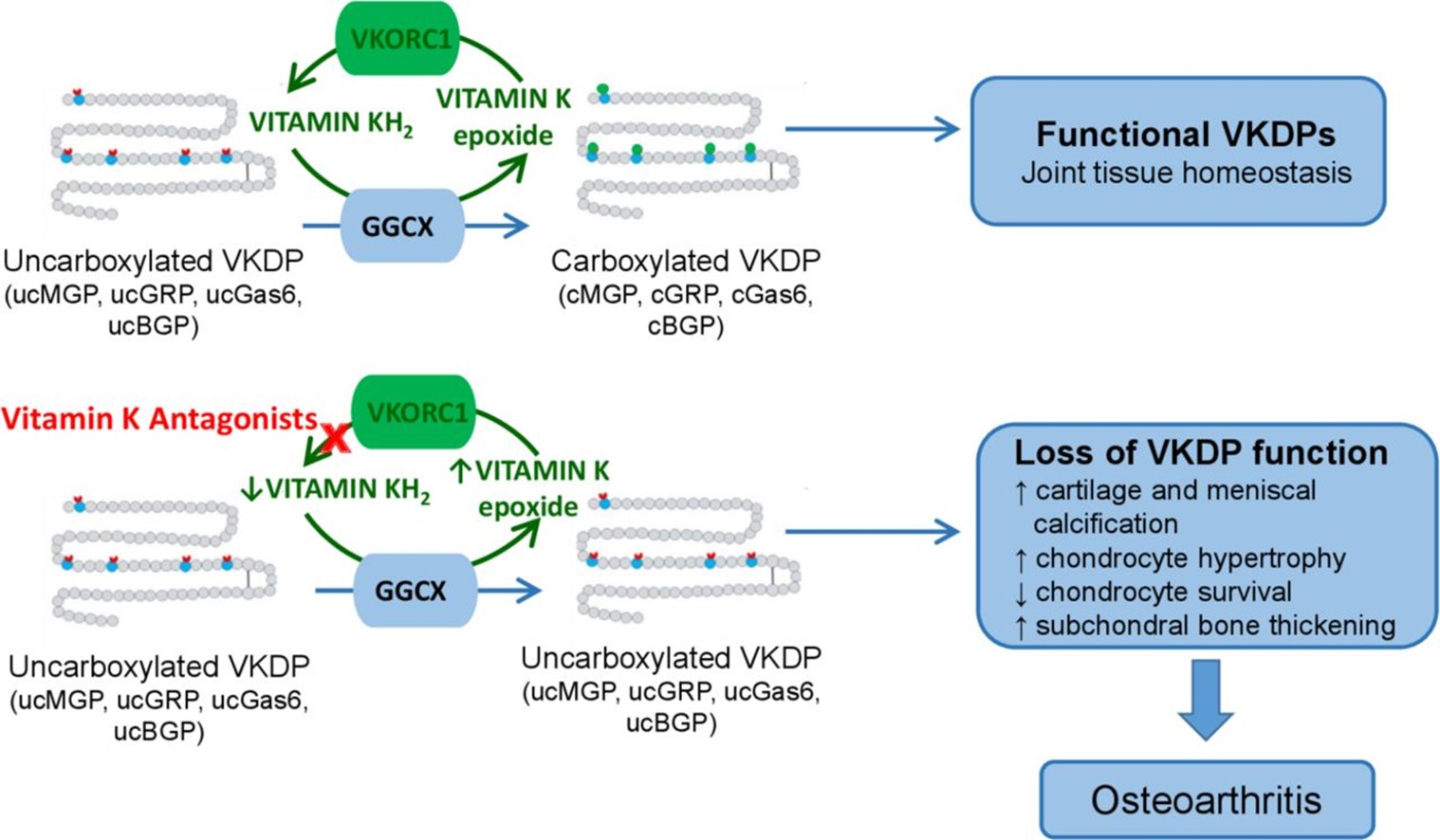
Hopefully, we evolve in our approach for activity recommendations and potentially pain management in groups that exhibit disabling conditions like osteoarthritis. I think this brings another point about the pathology of the two conditions and the relatedness. There has been evidence to support a vascular etiology and its ability to predict structural progression of osteoarthritis over 10 years (Jonsson et al., 2019; Wang et al., 2015). There is also data that relates use of statins to treat atherosclerosis and knee osteoarthritis progression (Clockaerts et al., 2012). Recently a nutritional link has been brought to light with Vitamin K and osteoarthritis. Vitamin K is commonly known for its role in blood coagulation (Loeser et al., 2021). Below is the figure Loeser et. al., uses to illustrate vitamin K role in osteoarthritis.
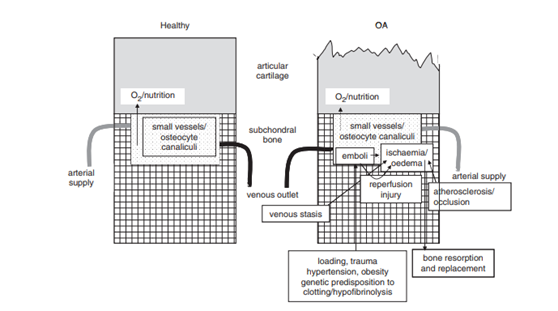
In the next figure below, Findlay 2007, shows how the subchondral vasculature is related to the initiation and/or progression of osteoarthritis. The left side shows healthy articular cartilage and the right side shows some cartilage erosion that may be related to changes due to an occlusion of blood supply.
References:
CDC, 2021. Benefits of Physical Activity [WWW Document]. Cent. Dis. Control Prev. URL https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm (accessed 5.20.21).
Clockaerts, S., Osch, G.J.V.M.V., Bastiaansen-Jenniskens, Y.M., Verhaar, J. a. N., Glabbeek, F.V., Meurs, J.B.V., Kerkhof, H.J.M., Hofman, A., Stricker, B.H.C., Bierma-Zeinstra, S.M., 2012. Statin use is associated with reduced incidence and progression of knee osteoarthritis in the Rotterdam study. Ann. Rheum. Dis. 71, 642–647. https://doi.org/10.1136/annrheumdis-2011-200092
Hall, K.S., Hyde, E.T., Bassett, D.R., Carlson, S.A., Carnethon, M.R., Ekelund, U., Evenson, K.R., Galuska, D.A., Kraus, W.E., Lee, I.-M., Matthews, C.E., Omura, J.D., Paluch, A.E., Thomas, W.I., Fulton, J.E., 2020. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int. J. Behav. Nutr. Phys. Act. 17, 78. https://doi.org/10.1186/s12966-020-00978-9
Jonsson, H., Fisher, D.E., Eiriksdottir, G., Aspelund, T., Klein, R., Gudnason, V., Cotch, M.F., 2019. Hand and knee osteoarthritis are associated with reduced diameters in retinal vessels: the AGES-Reykjavik study. Rheumatol. Int. 39, 669–677. https://doi.org/10.1007/s00296-019-04243-6
Liu, W., Balu, N., Canton, G., Hippe, D.S., Watase, H., Waterton, J.C., Hatsukami, T., Yuan, C., 2019. Understanding Atherosclerosis Through an Osteoarthritis Data Set. Arterioscler. Thromb. Vasc. Biol. 39, 1018–1025. https://doi.org/10.1161/ATVBAHA.119.312513
Loeser, R.F., Berenbaum, F., Kloppenburg, M., 2021. Vitamin K and osteoarthritis: is there a link? Ann. Rheum. Dis. 80, 547–549. https://doi.org/10.1136/annrheumdis-2020-219765
Skou, S.T., Pedersen, B.K., Abbott, J.H., Patterson, B., Barton, C., 2018. Physical Activity and Exercise Therapy Benefit More Than Just Symptoms and Impairments in People With Hip and Knee Osteoarthritis. J. Orthop. Sports Phys. Ther. 48, 439–447. https://doi.org/10.2519/jospt.2018.7877
Veronese, N., Stubbs, B., Solmi, M., Smith, T.O., Reginster, J.-Y., Maggi, S., 2018. Osteoarthristis Increases the Risk of Cardiovascular Disease: Data from the Osteoarthritis Initiative. J. Nutr. Health Aging 22, 371–376. https://doi.org/10.1007/s12603-017-0941-0
Vranish, J.R., Young, B.E., Stephens, B.Y., Kaur, J., Padilla, J., Fadel, P.J., 2018. Brief periods of inactivity reduce leg microvascular, but not macrovascular, function in healthy young men. Exp. Physiol. 103, 1425–1434. https://doi.org/10.1113/EP086918
Wang, Y., Dawson, C., Hanna, F., Fairley, J., Cicuttini, F.M., 2015. Association between popliteal artery wall thickness and knee cartilage volume loss in community-based middle-aged women without clinical knee disease. Maturitas 82, 222–227. https://doi.org/10.1016/j.maturitas.2015.07.010
Wolfe, A.S., Burton, H.M., Vardarli, E., Coyle, E.F., 2020. Hourly 4-s Sprints Prevent Impairment of Postprandial Fat Metabolism from Inactivity. Med. Sci. Sports Exerc. 52, 2262–2269. https://doi.org/10.1249/MSS.0000000000002367
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”