Shared Decision Making In Cardiac Care

Shared decision making (SDM) is an approach both patients and clinicians can use to improve patient education and discussion in decision making. Decision aids are tools that promote SDM by improving patient-clinician communication about all treatment options and how the risks and benefits fit with their personal values and preferences. Today, we’ll chat about SDM in the context of cardiac care, with examples from atrial fibrillation and heart failure, as well as the entire CAD spectrum.
A Chronological Look at SDM
In 2012, Karen Sepucha reflected on shared decision-making and patient decision aids in an editorial for Circulation: Cardiovascular Quality and Outcomes. Two studies published in the same issue evaluated the impact of decision aids in urgent management of acute coronary syndrome (The Chest Pain Choice Decision Aid) and vascular access choice for coronary angiogram procedures. These studies reflect scenarios that are not traditionally thought to be amenable to SDM, but the results show that SDM in the emergency department and regarding technical treatment decisions, such as femoral versus radial access, had a positive impact on patient knowledge and decisional conflict. Sepucha’s concluding statement still rings true today: “Despite considerable evidence from many studies of decision aids, few of these tools are used routinely in practice.”
There are several challenges to using decision tools in practice. Decision aids should be brief and easily incorporated into the workflow of clinical practice, as well as easily accessible in the public domain. In 2015, CMS implemented a policy around healthcare for atrial fibrillation patients requiring all non-implanting physicians to use evidence-based decision tools and SDM practices. A 2017 article by Megan Coylewright and David Holmes in Circulation caution against this CMS mandate for SDM for patients with atrial fibrillation. The authors cite reasons reminiscent of Sepucha’s conclusions in 2012. Coylewright and Holmes point out that there is limited guidance on navigating SDM for patients with atrial fibrillation at risk for stroke. Specifically, while research consistently shows that “decision aids improve patient outcomes including knowledge, engagement, and satisfaction”, SDM has yet to become an integral part of clinical practice for a variety of reasons, both on the patient side and the clinician side. For example, barriers to use of SDM by physicians include insufficient training in the skillsets necessary to implement SDM, such as “inadequate assessment of patient preferences,” in addition to logistic challenges to implementation, whether at the institutional level, the lack of publicly available decision aids, or the time availability during patient-clinician interactions to thoroughly discuss patient preferences.
Atrial Fibrillation
Atrial fibrillation presents a particularly challenging case for optimizing treatment, due to low prescription, low adherence due to side effects and frequent testing, as well as increased risk of negative reactions due to polypharmacy. Thomson et al. found that atrial fibrillation patients at risk of stroke may deicide to forgo treatment with anticoagulants to avoid the medications’ adverse effects, with the knowledge that their stroke risk later on increased. However, professional guidelines on treatment of atrial fibrillation promote SDM and use of evidence-based decision tools while recognizing that inviting patients to participate in care decisions can be challenging to physicians.
A recent systematic review, “Availability of Patient Decision Aids for Stroke Prevention in Atrial Fibrillation” by O’Neill and colleagues summarize the current state of decision aids for patients with atrial fibrillation at risk for stroke and their treating physicians. The current landscape of pharmacologic therapy for stroke reduction includes multiple DOACs, implantable LAA closure devices, aspirin, and warfarin – each treatment with benefits and trade-offs that must be considered “in the context of individual values and preferences and willingness to adhere to therapy”. Many of the decision aids in the studies reviewed by O’Neill et al. did not display all therapeutic choices, were delivered to patients primarily by nonphysicians, and were not publicly available.
Depression and CAD
SDM and decision tools pair nicely with assessment of depression in heart disease patients. In a recent paper, “Identifying and Managing Depression in Patients with CAD,” Aimee Salzer Pragle and Susan Salashor discuss the epidemiology and risk factors, clinical presentation, assessment tools, and treatment options for depression in patients with heart disease. In a 2011 review, Christopher Celano and Jeff Huffman estimated that 20-40% of patients with CAD may suffer from depression, and despite the availability of screening tools brief enough for clinical practice (such as the Patient Health Questionnaire-9 or -2), depression often goes unrecognized in cardiac care. Depression in patients with CAD is associated with progression of heart disease, poor quality of life and physical functioning, repeat cardiac events, and 2-2.5 fold increased risk of mortality [link]. Risk factors for depression in patients with CAD include “younger age, female sex, a history of depression, social isolation, previous cardiac events, and diabetes” and depression can increase risk of suicide, homicide, and substance abuse (which can exacerbate cardiac symptoms and promote further degeneration).
Innovative Frameworks – A Segue to Implementing SDM?
From the clinician side, disease-specific evaluation frameworks inclusive of all relevant aspects of a patient’s health provide another avenue towards optimizing patient-clinician communication. For example, in a recent paper, Gorodeski et al. present a multi-domain framework for managing heart failure and the associated questionnaires and tools that go with each task.
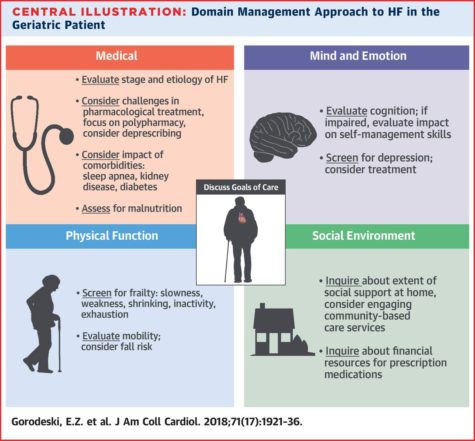
These tools include the Mini Nutritional Assessment Short Form (MNA-SF), the Mini-Cog and PHQ-2 (Patient Health Questionnaire) for mental and emotional state, gait speed, timed Up and Go test, FRAIL questionnaire, and ADL/IADL discussion for assessing physical function, as well as inquiries to social support at home, adaptable and safe environment plans, access to nutrition and transportation, as well as abilities and support in medication management (Table 1, Gorodeski et al).
Does your department or institution use shared decision making or decision aids in practice?
What barriers to implementation do you see in incorporating these tools into everyday patient interactions?
SDM and Decision Aids Resources
The Ottawa Hospital Research Institute hosts an up-to-date A to Z inventory of patient decision aids, and includes tools for angina, atrial fibrillation, CABG and other cardiac procedures, blood pressure medications, peripheral artery disease surgery, type 2 diabetes, depression, kidney disease and dialysis, and many others. Many of the tools geared towards cardiac care were in the form of informative articles for patients to read, or interactive tutorial-style pages for patients. None that I found were visual or brief enough to be used in clinical practice. Additionally, purely text-based “decision aids” are not useful for low-literacy populations, and online-only resources are not easily accessible for patients who are less tech-savvy. However, the Heart to Heart tool developed by the University of North Carolina General Internal Medicine department provides a user-friendly interface, even for the less technologically-savvy patients, that guides the user through several slides on how to join the discussion of their own treatment with their doctor. Similarly, the AHA Rise above Heart Failure initiative has two resources heart failure patients and physicians might find particularly useful: a guide to overcoming barriers to shared-decision making and a list of questions to ask the doctor. If you are a physician, reviewing these materials provides you with the guidance of what questions and topics to address during the clinic visit.
Quick links to select decision aids related to heart disease:
- Angina Treatment – Stents, Drugs, or Lifestyle Changes? (MayoClinic)
- Should I Take an Anticoagulant? (Healthwise)
- “ACE Inhibitors” and “ARBs” to Protect Your Heart? (AHRQ)
- Coronary Artery Disease: Should I Have Bypass Surgery? (Healthwise)
- Surgery for Peripheral Artery Disease (Healthwise)
- Type 2 Diabetes: Controlling Your Glucose by Taking a Second Medicine (NICE, UK)
- Rise Above Heart Failure: Questions to Ask Your Doctor (AHA)

Bailey DeBarmore is a cardiovascular epidemiology PhD student at the University of North Carolina at Chapel Hill. Her research focuses on diabetes, stroke, and heart failure. She tweets @BaileyDeBarmore and blogs at baileydebarmore.com. Find her on LinkedIn and Facebook.