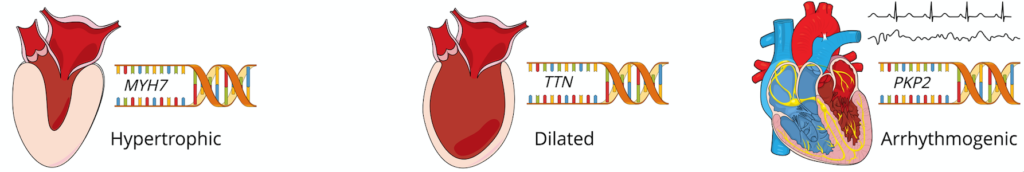
During my general cardiology fellowship, I developed a special interest in the care of patients with inherited cardiovascular disease. By virtue of the robust clinical activity of my division’s advanced heart failure and electrophysiology programs, I was exposed to clinical dilemmas like risk stratification in hypertrophic cardiomyopathy, primary prevention of sudden cardiac death in lamin A/C cardiomyopathy, and timing of heart transplantation for Danon disease early in my training. Refreshing my knowledge of clinical genetics alone was overwhelming, and I realized that while the rapid growth in genomic technologies was transforming our understanding of inherited cardiovascular disease, frontline clinicians were lagging behind in applying this knowledge to disease prevention and clinical care. To cultivate my interests further and learn to bridge this gap, I joined my institution’s new National Human Genome Research Institute (NHGRI)-supported postdoctoral training program in genomic medicine, a program created to prepare the next generation of physicians and scientists to implement genomic approaches to improve healthcare.
For M.D./D.O. trainees who have spent six consecutive years entrenched in clinical residency and fellowship programs, the idea of extending training by two years, re-entering the world of formal coursework and letter grades, and learning new skills to perform complex and unfamiliar research is more than enough to deter one from pursuing this career development track. However, participating in this program has afforded me many unexpected benefits outside the bounds of my clinical and research training:
- Caring for patients with a new type of multidisciplinary team:
- During my clinical training, my idea of a multidisciplinary care team was mostly grounded in my inpatient experience. While cooperating toward the same goal, physicians, nurses, advanced practice providers, therapists, nutritionists, pharmacists, social and case management workers often performed their roles asynchronously with little collaboration outside of the prescribed morning rounds. In contrast, my experience in our inherited cardiovascular disease clinic introduced me to a new paradigm essential to caring for patients and families with genetic disorders. I have been fortunate to learn about variant adjudication, pre-test and post-test counseling, cascade screening, and much more from our tremendous genetic counselors who are integral in the outpatient evaluations of our probands.
- Though the initial years of my practice have been focused in adult medicine, I have learned about the importance of tracking variant segregation in families and of comprehensive transitions of care through our joint familial cardiomyopathy and arrhythmia programs, partnerships with our neighboring pediatric hospital.
- Finally, I have witnessed the potential of real time bedside-to-bench-to-bedside research collaborations as shown by my mentors in their recent report of a clinical incorporation of rapid functional annotation of cardiomyopathy gene variants.1
- Developing and sharing expertise:
- In leading my fellowship’s didactic education curriculum as Chief Fellow, I took advantage of opportunities to share my new knowledge and skills with other fellows and residents. For our “fresh case” presentations, I often chose to present perplexing cases of cardiomyopathy to reinforce teaching points regarding the workup of genetic cardiomyopathies and the importance of taking a minimum three-generation family history.
- After completing the Examination of Special Competence in Adult Echocardiography, I led a fellow teaching conference on echocardiography in hypertrophic cardiomyopathy. I also joined our internal medicine residents for a clinicopathologic conference as an expert discussant, a position usually reserved for faculty but generously offered to me given my interest in cardiovascular genetics and enthusiasm for teaching.
- Pursuing these opportunities to develop and share my expertise has helped me solidify my own knowledge in the field, develop my oral and written communication skills, and grow as a peer mentor.
- Meeting physicians and scientists outside of cardiovascular medicine:
- The world often feels quite small while training within a medical specialty, but through my postdoctoral program, I have been exposed to physicians, scientists, and trainees in many disciplines outside of cardiovascular medicine. I heard diverse perspectives in my bioinformatics, biostatistics, and bioethics courses that have encouraged me develop my own independent opinions about my fields of interest. Multidisciplinary forums like genetics journal clubs, genetic rounds, and campus retreats have helped me contextualize the practice of genomic medicine.
My time in the postdoctoral program has shown me that these unexpected benefits of training are highly valuable to a trainee’s success. Through the genomic medicine postdoctoral program, the NHGRI “hopes to bring cross-training opportunities to individuals at different career levels and to support the training of investigators working in both basic genome science and genomic medicine” as it recognizes that this “is essential to realizing the full potential of genomics.”2
References:
- Lv W, Qiao L, Petrenko N, Li W, Owens AT, McDermott-Roe C, Musunuru K. Functional Annotation of TNNT2 Variants of Uncertain Significance With Genome-Edited Cardiomyocytes. Circulation. 2018;138(24):2852-2854.
- Green, Eric D. “NHGRI’s Research Training and Career Development: Genome Science to Genomic Medicine.” National Human Genome Research Institute. 3 Sept. 2014. https://www.genome.gov/27557674/may-5-nhgris-research-training-and-career-development-genome-science-to-genomic-medicine/