 I was in the mall one day and the saleswoman started talking about her health issues. For starters, I am not sure why she entrusted me with this information, but okay. So why is that conversation interesting enough to write about? Well, the lady was 20 years of age and she had undergone several cardiovascular challenges, including a cardiac ablation. I had heard of other people having this procedure done but I had not thought much about it (I looked it up but not in much detail), until I met this young lady. So, I started wondering:
I was in the mall one day and the saleswoman started talking about her health issues. For starters, I am not sure why she entrusted me with this information, but okay. So why is that conversation interesting enough to write about? Well, the lady was 20 years of age and she had undergone several cardiovascular challenges, including a cardiac ablation. I had heard of other people having this procedure done but I had not thought much about it (I looked it up but not in much detail), until I met this young lady. So, I started wondering:
- What is the underlying pathology that causes one to need to have the procedure?
- What is the average age of patients undergoing the procedure?
- What is cardiac ablation?
- How commonly is this procedure done?
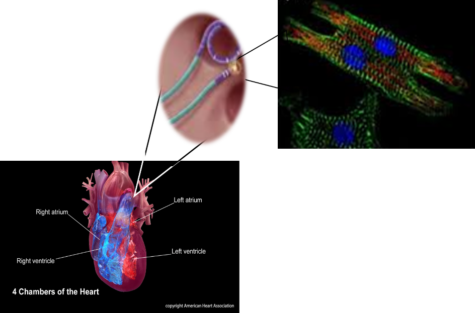
Cardiac ablation is the use of catheters to target and kill off specific cells within the heart, generally in the atrium. The adult mammalian myocardium has a negligible ability to regenerate once damage has occurred. Thus, rather than undergoing cardiomyogenesis (the formation of myocardium/heart muscles), fibrous tissue is instead formed. This phenomenon raised more questions for me, so I did literature searches…then more literature searches…then read more literature. The more I read, the more I felt I needed to read to understand why cardiologist would choose this procedure. Following a myocardial infarction (heart attack) a significant number of cardiomyocytes die leading to an enhanced inflammatory reaction. This cardiac event results in dead myocardial tissue being replaced with interstitial and perivascular collagen deposition. The presence of fibrosis can lead to pressure overload, increased blood pressure or potentially aortic stenosis. However, a patient that has suffered from myocardial infarction would not be a good candidate for cardiac ablation. So, who would be a good fit to undergo such a procedure? Usually it is a patient exhibiting cardiac arrhythmias, including atrial fibrillation (AF or AFib), supraventricular tachycardia (SVT), and Wolff-Parkinson-White Syndrome (WPW). Because this subject is enormous, I will only focus on AF due to the fact that it is the most common cause of arrhythmias treated with catheter ablation.
Pathophysiology of Atrial Fibrillation
AF is characterized by an abnormal heartbeat (quivering or irregular heartbeat) that causes the heart to ineffectively move blood into the ventricles. The onset of AF could be due to family history (genetics), but controllable risk factors are hypertension and valvular heart disease. The cardiovascular consequence of AF includes:
- Coronary artery disease
- Mitral stenosis
- Mitral regurgitation
- Left atrial enlargement
- Hypertrophic cardiomyopathy
- Congenital Heart Disease
- Cerebrovascular Accident
AF is considered the most common arrhythmic disease and it affects about 4% of the population. The prevalence of AF increase with age (<0.2% under 50 year of age (yoa), 4% are 60-70 yoa, and ~15% >80 yoa), with patients suffering from it has an average age between 75-85 yoa. In the U.S., there was a significant number of deaths (>200,000) resulting from AF in 2015, which is reason enough to pursue aggressive therapies to control this heart rhythm disorder.
Treatment
The European Society of Cardiology (ESC) released guidelines that summarized the current evidence that is available to physicians in selecting the best strategy for managing diseases, taking into consideration the risk-benefit ratio of diagnosis and therapeutic means. The recommended guidelines has shifted to focus on the identification of ‘truly low-risk’ patients (<65 with AF alone that does not need antithrombotic therapy) rather than ‘high-risk’ patients. Based on the earlier guidelines for treating AF, a patient of age >20 would not be considered for ablation therapy, so I wondered…what are the alternative treatments? I found they can either be drugs, such as: 1) Novel oral anticoagulants (blood thinners) fall into two categories (Oral direct factor Xa inhibitors or Oral direct thrombin) and 2) Left atrial ablation—introduced by American College of Cardiology Foundation, American Heart Association, and the Heart Rhythm Society.
To read more about these treatment, please be directed to European Heart Journal for the ESC Guidelines. Here I will focus on cardiac ablation.
Cardiac Ablation
 The normal mammalian heart is composed of tight layers of myocytes that are separated by small clefts creating a matrix network. The cardiac matrix network is divided into three constituents. The matrix network is collagen-based and serves as a scaffold for various components of the cell as well as transmission of contractive forces that keep the cells in correct timing with neighboring cells. When the heart undergoes damage, the resulting fibrosis disrupts the coordination of this myocardial excitation-contraction leading to hypertension. Subsequently, loss of collagen impair transduction, which causes the uncoordinated contraction of the cardiac muscle bundles (the quivering or fluttering that is felt with AF) or generation of re-entry circuits (irregular heartbeat).
The normal mammalian heart is composed of tight layers of myocytes that are separated by small clefts creating a matrix network. The cardiac matrix network is divided into three constituents. The matrix network is collagen-based and serves as a scaffold for various components of the cell as well as transmission of contractive forces that keep the cells in correct timing with neighboring cells. When the heart undergoes damage, the resulting fibrosis disrupts the coordination of this myocardial excitation-contraction leading to hypertension. Subsequently, loss of collagen impair transduction, which causes the uncoordinated contraction of the cardiac muscle bundles (the quivering or fluttering that is felt with AF) or generation of re-entry circuits (irregular heartbeat).
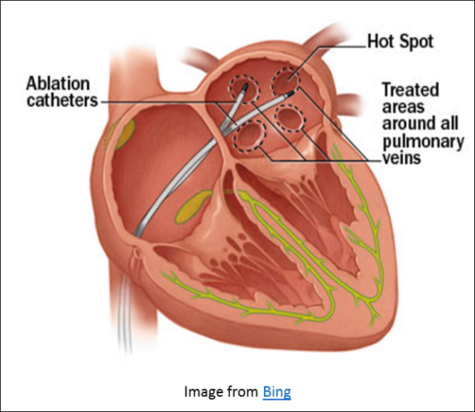
The ablation process will depend on the patient medical condition, past cardiac history, and the ablation technique chosen. There are several types of catheter ablation
a) Radiofrequency ablation-use radiofrequency generators to deliver a current, in a point by point fashion around the pulmonary vein, creating a circular scar around each vein.
b) Cryoablation—uses a single catheter that travels through the femoral vein in the groin to the left atrium. The balloon end (halo) of the catheter has a refrigerant that freezes the tissue it comes in contact with creating a scar.
c) Surgical ablation—generally used when open heart surgery is being conducted.
i. Mini Maze-use 3-5 incisions on the front and side of the chest to insert the catheter to freeze/heat cardiomyocytes
ii. Convergent—uses both surgical and catheter based techniques.
Catheter ablation is generally an outpatient procedure, but it should not be taken lightly. As with most consumers, cost comes to mind. How can cardiologist/electrophysiologist conduct such a procedure in so short of a time and charge so much? The answer is simple. The technology used in ablation is extensive; mapping equipment, cardioverter/defibrillator and catheter, recording apparatus, stimulators, and junction boxes. I am overwhelmed just thinking about it all!
Wrap it up…
Cardiovascular disease is a consequence of a lot of factors. Understanding the various procedures that the cardiologists are explaining can be daunting. Even with the expansive literature that is available it is difficult to determine how a procedure will work for each patient, especially with regard to the side effects. For example, in a 2010 study for rhythmic control (294 patients), there was no significant difference between patients that received the catheter ablation compared to those taking antiarrhythmic drugs as a first line of intervention. Catheter ablation is said to be more effective than antiarrhythmic drugs, but the recurrence of AF is significant during long term follow up. Early recurrence of AF is the best predictor of whether one will have a recurrence later. In an observational study conducted at high volume clinics, there was a 39% hospitalization rate post catheter ablation. However, catheter ablation has been deemed reasonable for first line of therapy for AF when patients have paroxysmal AF and low risk for procedures with complications; which is interesting since the majority of studies are inherently biased toward the experienced centers. It is reasonable to speculate that people, such as the saleswoman in the mall, who visit small low volume clinics, contribute to increased rates of hospitalization rates.
I am, furthermore interested in knowing whether there is a decrease in cardiac output post catheter ablation. If this procedure is killing off specific cells in the heart and leaving scar tissue, what are the downstream effects of this cardiac cell death? Especially in patients that have repeated catheter ablations. If there is a decrease in cardiac output, and the kidney filters 20% of the cardiac output daily, then what effect does cardiac ablation have on the renal system? Could this procedure enhance renal failure? I have had conversations with other people who have had cardiac ablations that later suffered from renal failure necessitating dialysis. Since all conditions are patient specific, there is no evidence that catheter ablation is connected to renal failure to my knowledge, but I wonder if anyone else had that observation.
To sum up the conversation I had with the young lady in the mall. She started her cardiac journey at an early age. She has gone through oral anticoagulant drugs, catheter ablation, and open-heart surgery. By the age of 20, that is a lot for one to have gone through. She was in such distress about having to undergo yet another catheter ablation that she was seeking answers to help her understand what she was going through and how to make informed decisions about her care. How can patients be better educated on what is going on with their bodies when visiting medical professionals? People are told to take responsibility for their care, but what if they do not understand enough to know what to ask?

Anberitha Matthews, PhD is a Postdoctoral Fellow at the University of Tennessee Health Science Center in Memphis TN. She is living a dream by researching vascular injury as it pertains to oxidative stress, volunteers with the Mississippi State University Alumni Association, serves as Chapter President and does consulting work with regard to scientific editing.