The COVID-19 pandemic has skyrocketed many fields of healthcare – basic science research, outcome-based research, and epidemiological factors affecting healthcare. We already know obesity affects >4 in 10 adults in the United States and contributes to diabetes, heart disease, ultimately leading to increased morbidity and mortality1. Based on prior experience, we have learned that obesity is associated with an increased risk of other respiratory viruses, such as influenza. These same patients tended to have a higher risk of hospitalization and death, along with longer lengths of stay and mechanical ventilation compared to patients who have normal weight2.
In January of 2021, researchers used the American Heart Association’s COVID-19 Cardiovascular Disease Registry to look at the effect of obesity across different groups’ mortality, need for mechanical ventilation or both. Analysis of data from 88 hospitals in the US showed that classes I to III obesity were associated with a higher risk of in-hospital death or mechanical ventilation compared to normal weight when these patients are hospitalized with COVID-19. The association was strongest in adults <50 and weakest in adults >70 years of age. This was the first study to show the harmful effects of obesity on COVID-19 outcomes may be limited to people under 50 rather than those that are older and obese. There could be a number of reasons for this observation – including comorbid conditions such as diabetes, hypertension, or even delays in seeking care3. As a critical care provider, this study definitely made me evaluate risk factors for younger patients (and even family members) differently.
In a time where one study is not simply the end-all-be-all, a more recent study from the United Kingdom had a similar message. The study was led by Nuffield Department of Primary Care Health Sciences and had 6.9 million patients – which is an outstanding number! And what did they discover??
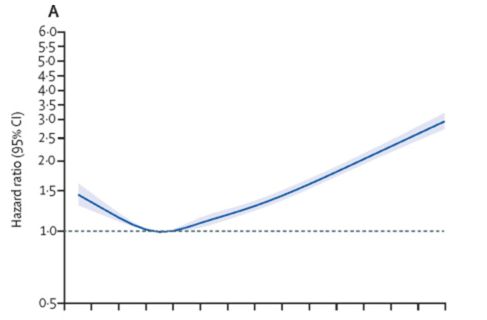

Figure A shows patients with low BMI (<18.5) had an increase in COVID-19 related admissions to the ICU along with a steady increase in admissions to the ICU as the BMI increased. Figure B shows a linear association across the whole BMI range for death due to COVID-194. Dr. Carmen Piernas, lead author of the study said: “Our Study shows that even very modest excess weight is associated with greater risks of severe COVID-19 complications and the risks rise sharply as BMI increases. Also, risks associated with excess weight are greatest in people <50 years, while weight has little to no effect on your chances of developing severe COVID-19 after age 80. These findings suggest that vaccination policies should prioritize people with obesity.” The impact of obesity was most marked in people in the youngest age range of 20-39. The study shows that obesity is not only a chronic disease but also a risk factor for acute illness or death. Taking it one step further, health care providers across the spectrum will have to work harder to help provide evidence-based treatments for patients to help reduce their weight.
One of the most striking aspects of this study was the number of patients they tracked in the outpatient setting who ended up needing to go to the hospital. They tracked these patients in their disease course in hopes of giving us information for people in the general community rather than those already admitted to the hospital. At this time, there is no study looking to see if weight reduction specifically reduces the risk of severe COVID-19 outcomes, but I would be interested in such a study.
There was also a significant interaction between BMI and self-reported ethnicity for hospital admissions and death due to COVID-19, with Black people having a higher risk than white people. It’s unclear as to why this association exists in a country where all the citizens have free access to healthcare. There are a few hypotheses but nothing concrete has been established.
Overall, with the addition of this large study plus what we have known before, we can be confident that obesity continues to have significant health implications. I hope we never see another pandemic but if we do, I’m confident what we have learned over the past year will help us treat our patients more efficiently and effectively.
References
- Romero-Coral A, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancent. 2006;368:666-678.
- Jain S, Chaves SS. Obesity and influenza. Clinic Infect Disease. 2011;53:422-424.
- Hendren N, et al. Association of body mass index and age with morbidity and mortality in patients hospitalized with COVID-19 results from the American Heart Association COVID-19 cardiovascular disease registry. Circ. 2021;143:135-144
- Gao M, et al. Associations between body-mass index and COVID-19 severity in 6.9 million people in England: a prospective, community-based, cohort study. Lancet. 2021;
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”