As we continue to see the increasing number of coronavirus disease 2019 (COVID-19) cases and amid the second peak of this pandemic in the United States (US), everyone from physicians to the general public should know how to approach and perform basic life support (BLS) with certain precautions and modifications of routine BLS protocols for patients with suspected or confirmed COVID-19 status. Importantly, rescuers should always balance the immediate needs of patients with their own safety. Several recently published articles have demonstrated that many patients with COVID-19 can present with cardiac arrest or experience cardiac arrest while hospitalized. In this post, I am going to share a few points on recommended modifications in order to ensure a safe yet effective CPR protocol for our patients.
- Reduce Provider Exposure to COVID-19
Resuscitations carry added risks to rescuers and healthcare workers for many reasons. CPR involves performing numerous aerosol-generating procedures, including chest compressions, positive-pressure ventilation, and establishment of an advanced airway [1]. It is important to keep in mind that these viral particles can remain suspended in the air with a half-life of around 1 hour per some reports and can be inhaled by those nearby [1]. In addition, resuscitation efforts require numerous providers to work in close proximity to each other and to the patient; thus, the advised social distancing protocols may not be applicable.
Strategies
- Before entering the scene, all rescuers should don personal protective equipment (PPE) to guard against both airborne and droplet particles.
- Limit personnel on the scene to only those essential for patient care.
- In settings with protocols in place and expertise in their use, consider replacing manual chest compressions with mechanical CPR devices to reduce the number of rescuers whenever it is available and in patients who meet the manufacturer’s height and weight criteria.
- It is important to clearly communicate the COVID-19 status to anyone arriving to the scene and when transferring patients to another setting.
- Prioritize Oxygenation and Ventilation Strategies with Lower Aerosolization Risk
Strategies
- Attach a high-efficiency particulate air (HEPA) filter securely [Figure 1], if available, to any manual or mechanical ventilation device to lower the risk of aerosolization before giving breaths.
- After healthcare providers assess the rhythm and defibrillate any ventricular arrhythmias, patients in cardiac arrest should be intubated with a cuffed tube at the earliest feasible opportunity. Connect the endotracheal tube to a ventilator with a HEPA filter when available.
- Minimize the likelihood of failed intubation attempts by doing the following:
- Assign the provider/approach with the best chance of first-pass success, and
- Pause chest compressions while intubating with minimal disruption.
- Video laryngoscopy may reduce exposure to aerosolized particles and should be considered.
- Once on a closed circuit, minimize disconnections in order to reduce aerosolization.
- Barriers can be used to minimize spread of the particles during aerosol-generating procedures (Figure 2).
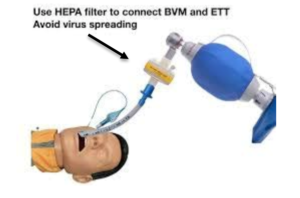
Figure 1: A high-efficiency particulate air (HEPA) filter (arrow) is securely attached to any manual or mechanical ventilation device to lower the risk of aerosolization before giving breaths [2].

Figure 2: Example of barriers potentially used to minimize the spread of the particles during aerosol-generating procedures [2].
- Consider the Appropriateness of Starting and Continuing Resuscitation
Like any cardiac arrest, it is important to know when resuscitation efforts are likely to be futile. Although the outcomes for cardiac arrest in COVID-19 are still unknown, the mortality for critically ill patients with COVID-19 is high, especially with increasing age and comorbidities, particularly cardiovascular disease. As such, it is critical to consider all these factors in determining the appropriateness of initial and continued resuscitation efforts, to weigh the likelihood of success against the risk to rescuers.
Strategies
- Address goals of care with patients, or their proxies, in anticipation of the potential need for increased levels of care.
- Healthcare systems and Emergency Medical Services (EMS) agencies should institute policies to guide frontline providers in determining the appropriateness of starting and terminating CPR for patients with COVID-19 on the scene, early in the process. The risk stratification and potential policies should be communicated to patients (or proxy) during discussions of goals of care.
In conclusion, there have been modifications to the routine CPR protocols in patients with suspected or confirmed COVID-19. With the increasing number of COVID-19 cases, it is very important, for us as physicians and for the general public as well, to review recommended modifications to BLS protocols and apply them where possible, in a step to win the battle against this virus during these unprecedented times!!
References
- Edelson DP, Sasson C, Chan PS, et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141(25):e933-e943. doi:10.1161/CIRCULATIONAHA.120.047463 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7302067/
- Medical Direction and Practice Board White Paper Approach to Out-of-Hospital Cardiac Arrest During the COVID-19 Pandemic: https://www.maine.gov/ems/sites/maine.gov.ems/files/inline-files/2020-04-30%20OHCA%20COVID-19%20White%20Paper%20Final.pdf
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”