In recent years, the role of intestinal microbiome and host health has gained wide interest due to many findings suggesting gut microbiota may play a role in the development and maintenance of cardiovascular disease (CVD) and metabolic disorders, such as hypertension, obesity, diabetes mellitus, and metabolic syndromes. Hypertension, one of the important risk factors for CVD, plays a significant role in intestinal dysbiosis. Dysbiosis is a change in the gut microbiota that imbalance the ratio of Firmicutes (F) to Bacteroidetes (B) (F/B) and is considered as a biomarker for gut dysbiosis. When environmental factors, dietary habits, medications such as antibiotics, intestinal infections or other factors alter the species and balance of the intestinal microorganism ecosystem in the adult gut, dysbiosis can take place, causing inflammation and metabolic disorders, thus promoting the development of CVD.
The recently discovered contribution of intestinal microbiota and its contribution to the development of CVDs and its risk factors has significantly increased attention to the important connection between the heart and the gut. The intestinal microbiota function as a filter of our largest environmental exposure, that is what we eat. What we eat provides nutrients for intestinal microbial metabolism. Several intestinal microbial metabolites are biologically active and could possibly affect the host phenotype and health outcomes.
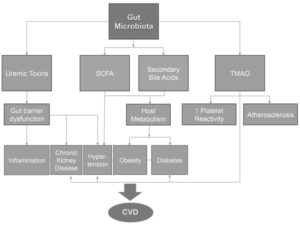
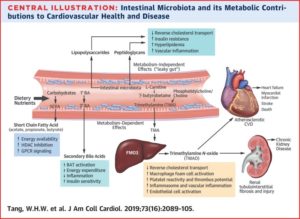
The gut microbiota resembles a large virtual endocrine organ that is capable of responding and reacting to circulating signaling molecules within the host. Intestinal microbiota- host interaction occurs through many pathways, including trimethylamine-N-oxide (TMAO) and short chain fatty acids (SCFA). This interaction has been shown to affect the host phenotypes relevant to cardiovascular disease, ranging from inflammation, obesity, and insulin resistance, to more direct process like atherosclerosis and susceptibility to hypercoagulability. Furthermore, multiple animal and human clinical studies revealed striking association between either gut microbiota composition, or their derived metabolites, and both the presence and incident development of CVD.
The healthy gut microbiome
The composition of the healthy gut microbiome can vary significantly across individuals. However, this composition is relatively stable over time. The gut microbiome is primarily composed of species within the Bacteroidetes, Firmicutes, Actinobacteria, Proteobacteria and Cerrucomicrobia phylae. The precise composition of species varies among individuals due to variety of genetic and environmental factors, including diet and medications used such as antibiotics. It is not surprising that microbial metabolite profiles are strongly associated with enterotypes. For instance, Bacteroidetes bacteria predominantly metabolize proteins, whereas, Prevotella species are saccharolytic bacteria that primarily metabolize carbohydrates. The gut microbiota has evolved to play a symbiotic role in extracting calories from indigestible macromolecules. Indigestible carbs and proteins are fermented by the colonic bacteria to form short chain fatty acid (SCFA) such as acetate, propionate and butyrate which play a significant role in weight loss and provide various health benefits. Microorganisms that are incapable of catabolism of indigestible macromolecules, use the SCFA produced by other microbiota as fuel in a process called cross-feeding. In addition to its role as an important energy source for both host and microbiota, the SCFA is important in regulation of the inflammatory response. Furthermore, commensal gut bacteria are necessary for dampening the immune response to non-pathogenic bacteria, hence they protect the host from the harms of sterile inflammation and they are also responsible for establishing an intact gut epithelial barrier, thus preserving the digestive and absorptive functions of the intestine and protecting from the invasion of pathogens and toxic metabolites into the circulation.
The Intestinal Microbiota and CVD:
The unique link between the gut microbiota and cardiovascular diseases has been described recently with the discovery of the link of Trimethylamine-N-Oxide (TMAO) to atherosclerosis. TMAO is produced by the breakdown of Phosphatidylcholine and other trimethylamine containing compounds by the intestinal bacteria. In a recent human experiment that consisted of ingestion of two hard boiled eggs (high in phosphatidylcholine) and deuterium [d9]-labeled phosphatidylcholine before and after suppression of intestinal microbiota with oral broad-spectrum antibiotics, it was found that circulating TMAO and its d9 isotopologue (both molecules are derived from the metabolism of phosphatidylcholine) was remarkably elevated after the phosphatidylcholine challenge. However, plasma levels of TMAO were markedly suppressed after the administration of antibiotics and then reappeared after withdrawal of antibiotics. In a large independent clinical cohort (n=4,007), patients in the highest quartile of plasma TMAO levels had a 2.5-folds higher risk of major adverse cardiovascular event than patients in the lowest quartile. Furthermore, higher fasting plasma levels were found to correlate with the risk of incident major adverse cardiovascular events independent of the classic cardiovascular risk factors. In mouse models, studies confirmed that dietary supplementation of Choline or TMAO increased TMAO levels, macrophage foam cell formation and inflammation, and atherosclerosis development. Moreover, TMAO has also been shown to enhance platelet hyperactivity and thrombosis risk. In a human cohort study, there was a dose-dependent association between plasma TMAO levels and platelets aggregation. This association explains the increased risk of cardiovascular events with high TMAO levels.
Ahmadmehrabi S, Tang WHW. Gut microbiome and its role in cardiovascular diseases. Curr Opin Cardiol. 2017;32(6):761-766. doi:10.1097/HCO.0000000000000445
Dysbiosis has been linked to increased CVD risk. A lower ratio of Bacteroidetes to Firmicutes has been associated with significantly increased risk to hypertension, diabetes mellitus, obesity and atherosclerosis. When there is decreased intestinal microbiota diversity (decreased Bacteroidetes to Firmicutes ratio) there will be an increase in the plasma TMAO levels and reduced SCFA level which is important for increasing insulin sensitivity, secretion of the satiety hormone GLP1, lower BMI and increase HDL levels. Higher levels of TMAO and lower levels of SCFA has been associated with increased risk for Type 2 Diabetes (T2DM) and metabolic syndrome. Hypertension has also shown to be associated with gut dysbiosis; however, the exact mechanism is still unknown.
Therapeutic Interventions:
The recent discovery of the TMAO and SCFA pathways and evidence for links between gut dysbiosis and several risk factors for cardiovascular disease now provides new opportunities for therapeutic interventions. Now knowing that alteration in the gut microbiota community is associated with much pathology, therapeutic interventions aimed at restoring microbial composition balance present an auspicious therapeutic approach. A fiber rich diet has been reported to increase SCFA- producing microbiota and lower blood pressure in patients with end-stage-renal disease. Dietary supplements of prebiotics, which are typically food indigestible molecules have a favorable impact on intestinal microbiota composition and can be beneficial. Similarly, probiotics, which are compilation of live bacteria administered to promote gut microbiome health have shown to have beneficial effects on the gut microbial environment and to be associated with cardioprotective effects. While prebiotics and probiotics focus on eliciting the growth of healthy gut bacteria, antibiotics treatment is focused on reducing the harmful bacteria content. However, the lack of specificity of broad-spectrum antibiotics makes them a less favorable approach.
With the recent discovery of the unique pathways between the gut microbiome and the heart and their association with CVD, we are presented with a new and a promising opportunity for CVD treatment and prevention. The most up-to-date discoveries and use of a structural analog of choline,3,3-dimethyl-1-butanol (DMB), was shown to inhibit TMA production and reduce circulating plasma TMAO levels and to reduce macrophage foam cell formation and risk of atherosclerosis, more importantly, this small-molecule inhibitor shown not be lethal to the gut microbiota ecosystem.
References:
- Ahmadmehrabi S, Tang WHW. Gut microbiome and its role in cardiovascular diseases. Curr Opin Cardiol. 2017;32(6):761-766. doi:10.1097/HCO.0000000000000445
- Yang T, Richards EM, Pepine CJ, Raizada MK. The gut microbiota and the brain-gut-kidney axis in hypertension and chronic kidney disease. Nat Rev Nephrol. 2018;14(7):442-456. doi:10.1038/s41581-018-0018-2
- Jin M, Qian Z, Yin J, Xu W, Zhou X. The role of intestinal microbiota in cardiovascular disease. J Cell Mol Med. 2019;23(4):2343-2350. doi:10.1111/jcmm.14195
- Tang WHW, Bäckhed F, Landmesser U, Hazen SL. Intestinal Microbiota in Cardiovascular Health and Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(16):2089-2105. doi:10.1016/j.jacc.2019.03.024
- Yoshida N, Yamashita T, Hirata KI. Gut Microbiome and Cardiovascular Diseases. Diseases. 2018;6(3):56. Published 2018 Jun 29. doi:10.3390/diseases6030056
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”