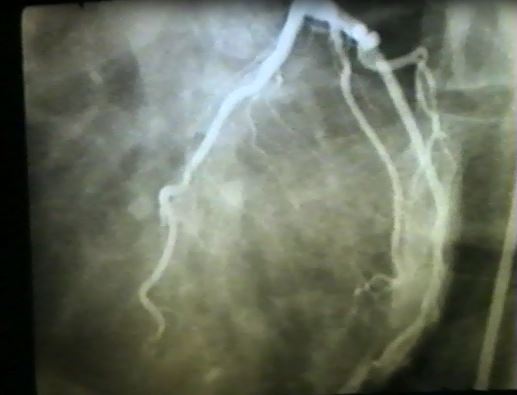
One of the most challenging clinical scenarios to a cardiologist is the patient presenting with symptoms suggestive of obstructive coronary artery disease (i.e. angina), in whom coronary angiography reveals patent coronary vessels. Due to the seemingly ‘normal’ arteries, current clinical practice tends to underestimate the impact of these presentations, but there are subsequent difficulties in their management. To many cardiologists, angina in the absence of CAD is a myth rather than a fact — “what you don’t know, you don’t miss.” One such presentation often being missed or ignored is the “coronary slow flow phenomenon.” A classic example of slow flow angiogram is shown here.
What is coronary slow flow?
Nearly 50 years ago, Tambe and colleagues1 initially described this angiographic entity in patients with angina symptoms where they noted the injected contrast during coronary angiography moved very slowly through the coronary arteries, and aptly named “coronary slow flow phenomenon.” The prevalence is estimated at approximately 1-7% of elective angiograms2,3. The condition was largely neglected until Professor John Beltrame identified the distinct clinical features associated with this intriguing entity and thus concluded the coronary slow flow phenomenon was a new coronary disorder rather than angiographic curiosity. Evidence suggests that the coronary slow flow phenomenon leads to clinical manifestations of ischemia, arrhythmias, acute coronary syndromes and even sudden cardiac death.
How is coronary slow flow diagnosed?
Coronary slow flow phenomenon is usually identified subjectively by visual judgment.
- Thrombolysis in myocardial infarction (TIMI) flow grade reflects the speed and completeness of the passage of the injected contrast through the coronary tree. In the setting of coronary slow flow, diagnosis can be made on the basis of TIMI 2 flow grade (ie: requiring ≥ 3 beats to opacify the vessel)4.
- Corrected TIMI frame count (CTFC) facilitates the standardization of TIMI flow grades and flow assessment. It represents the number of cine-frames required for contrast to first reach standard distal coronary landmarks. TIMI frame count > 27 frames have been frequently used to diagnose slow flow5.
What is the underlying cause of this presentation?
The coronary circulation consists of epicardial vessels and microvasculature. In the absence of epicardial stenosis, microvascular dysfunction may explain the pathophysiology of coronary slow flow phenomenon. Supporting this hypothesis, biopsy studies have revealed structural microvascular coronary abnormalities in slow flow patients. Reduced endothelium dependent flow-mediated dilatation (FMD) of the brachial artery has been detected in patients with coronary slow flow phenomenon, suggesting that endothelial dysfunction is implicated in the aetiology. However, there are still multiple questions and controversies regarding the underlying pathophysiology and whether this pathology is limited to coronary arteries or is a manifestation of systemic vascular or endothelial disease remains to be answered.
What is the medical management for coronary slow flow phenomenon?
Although coronary slow flow phenomenon patients have good overall prognosis, ongoing anginal episodes results in considerable impairment of their quality of life. Professor Beltrame has been long fighting the battle of identifying appropriate management for these patients, in particular, therapies that limiting the anginal episodes. His group has shown dipyridamole and mibefradil has some benefit in this setting, yet larger studies are required to confirm these findings. Currently available anti-anginal agents are of limited clinical value. To date, no large trial testing pharmacological approaches has been conducted, and the evidence available is derived from small studies, some with inhomogeneous inclusion criteria.
So, is it a myth or fact?
Over the past 50 years, the coronary slow flow phenomenon has evolved from a curious ‘myth’ to an identified coronary disease entity. Despite this progression of thinking, significant efforts are still required to unpack this intriguing condition, particularly in relation to effective therapies to improve symptoms and quality of life.
References:
- Tambe AA, Demany MA, Zimmerman HA and Mascarenhas E. Angina pectoris and slow flow velocity of dye in coronary arteries–a new angiographic finding. Am Heart J. 1972;84:66-71.
- Beltrame JF, Limaye SB and Horowitz JD. The coronary slow flow phenomenon–a new coronary microvascular disorder. Cardiology. 2002;97:197-202.
- Hawkins BM, Stavrakis S, Rousan TA, Abu-Fadel M and Schechter E. Coronary Slow Flow– Prevalence and Clinical Correlations &ndash. Circulation Journal. 2012;76:936-942.
- Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, Dodge HT, Francis CK, Hillis D, Ludbrook P and et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76:142-54.
- Gibson CM, Cannon CP, Daley WL, Dodge JT, Jr., Alexander B, Jr., Marble SJ, McCabe CH, Raymond L, Fortin T, Poole WK and Braunwald E. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996;93:879-88.