In our previous blogs, we discussed that doctors can diagnose Moyamoya disease using medical imaging systems, such as positron emission tomography (PET) and magnetic resonance imaging (MRI). But which one is better?
According to some recent studies performed by Dr. Moss Zhao (AHA Postdoctoral Fellow, 2021) at Stanford University, MRI is better thanks to its accessibility, safety, and affordability.
For decades, PET has been the gold standard technique for diagnosing Moyamoya disease based on imaging the blood flow in the abnormal blood vessels in the brain. However, PET uses radioactive tracers to create the images, making it complex and expensive. Although the amount of radiation is less than a 5-hour flight, doctors have sought for alternative and less invasive techniques to replace PET, especially for children. In recent years, arterial spin labeling (ASL), an advanced MRI technique, has emerged to replace PET imaging to measure blood flow in the brain. Because ASL MRI is more accessible at most hospitals and the procedure is less complex than PET, ASL has gained popularity in many research and clinical institutions for Moyamoya patients.
At Stanford University, Dr. Moss Zhao demonstrated that ASL could replace the conventional PET imaging technique without exposing patients to radiation and causing side effects. The image quality and measurement accuracy of ASL are compatible with PET, implying that ASL can be used to characterize the abnormal blood flow and circulation in Moyamoya patients. Among the different implementations of ASL, Dr. Zhao developed an advanced technique dubbed ‘multi-delay ASL’ that gives the best image quality with the least amount of scanning time. For less than 5 minutes, multi-delay ASL can produce images that require more than 20 minutes for PET imaging. The image in this blog shows the images collected by ASL and PET at the same time from normal and healthy people. Using the latest ASL techniques, doctors can identify patients with a high risk for stroke based on their MRI scans for just under 5 minutes without using any radioactive substances. Dr. Zhao’s team is currently testing this technique on the pediatric population to enable this non-invasive imaging technology to be accessible to patients across the lifespan.
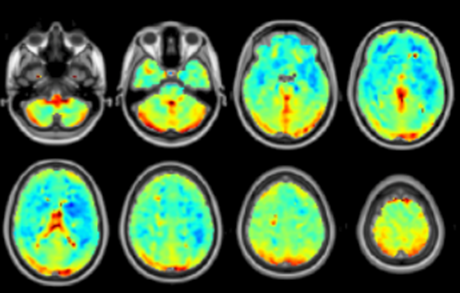
Image source: NeuroImage
References:
https://doi.org/10.1016/j.neuroimage.2021.117955
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”