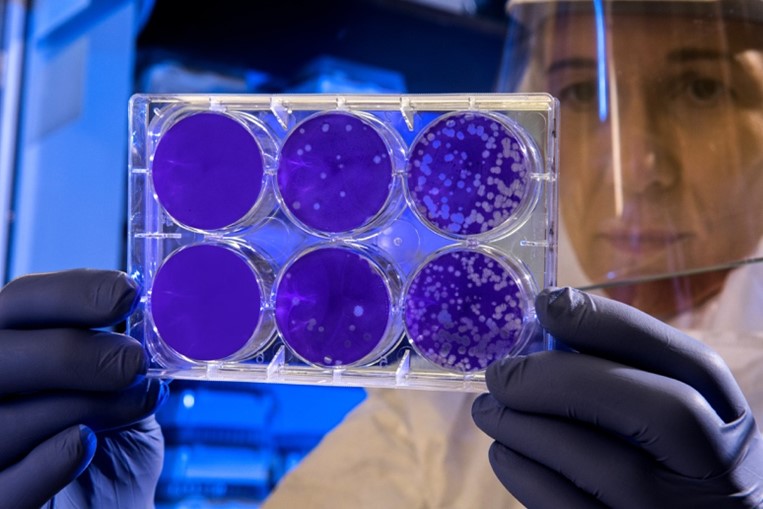
Photo by CDC on Unsplash
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), represents a global health crisis. Cough, fever, and shortness of breath are the most common reported symptoms; however, neurological and gastroenterological manifestations can also be present1. Angiotensin-converting enzyme 2 (ACE-2) has been shown to act as a co-receptor to facilitate coronavirus entry by efficiently binding to the S1 domain of spike protein, a surface glycoprotein of SARS-CoV2. The pathogenesis of COVID-19 depends on the localization of the coronavirus co-receptors. The epithelium of lungs and intestine is rich in ACE-2 expression, thereby providing a possible route of entry for SARS-CoV-2. Further, ACE-2 is also expressed on Type I and type II pneumocytes providing other entry sites for SARS-CoV-2. Virus entry can cause pathological changes at the alveoli-capillary interface. Additionally, copious expression of ACE-2 on the type II alveolar cells can promote rapid viral expansion resulting in further alveolar damage and hyperinflammation3,4.
ACE-2 is also present on endothelial cells, smooth muscle cells, and perivascular pericytes in all the organs, indicating that if SAR-COV-2 is transmitted to the blood circulation, the virus can quickly spread throughout the body3. The postmortem lung tissues of COVID-19 patients exhibited a higher number of ACE-2 positive endothelial cells and a higher prevalence of endothelial injury (disruption of cell membrane and presence of the intracellular virus) and microthrombi than lung tissues of patients who died from influenza-associated respiratory failure1,5. The most common comorbidities observed in COVID-19 patients are hypertension, diabetes, and obesity, all of which are associated with endothelial dysfunction. Further, COVID-19 patients are projected to be at a higher risk of deep vein thrombosis, systemic vasculitis, and acute pulmonary embolism6,7, possibly due to underlying endothelial cell injury and inflammation. Thrombi can directly affect gas exchange and cause and cause multisystem organ dysfunction in COVID-19 pneumonia8. Upon activation, platelets release polyphosphates, which accelerate the activation of factors V and XI, inhibit tissue factor pathway inhibitor and contribute to thicker fibrin strands synthesis. Further, the cytokine release can activate endothelial cells resulting in a prothrombotic environment1.
Acute respiratory distress syndrome is suggested to be caused by the dissociation between lung mechanics, loss of lung perfusion regulation and hypoxic vasoconstriction, and severe hypoxemia9. The loss of hypoxic vasoconstriction can be due to increased mitochondrial oxidative stress resulting in pulmonary endothelial cell dysfunction10. SARS-CoV-2 elements, accumulation of inflammatory cells, intracellular virus, and disrupted cell membranes are detected in the endothelial cells of COVID-19 patients5,11, further indicating endotheliitis /endothelial cell dysfunction during COVID-19 infection. Endothelial cell dysfunction can cause abnormalities in microcirculation in different vascular beds and contribute to life-threatening complications of COVID-19, including thromboembolism and multiple organ damage.
References:
- Huertas A, Montani D, Savale L, et al. Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)? Eur Respir J. 07 2020;56(1)doi:10.1183/13993003.01634-2020
- Ziegler CGK, Allon SJ, Nyquist SK, et al. SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues. Cell. 05 28 2020;181(5):1016-1035.e19. doi:10.1016/j.cell.2020.04.035
- Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. Jun 2004;203(2):631-7. doi:10.1002/path.1570
- Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 03 28 2020;395(10229):1033-1034. doi:10.1016/S0140-6736(20)30628-0
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 07 09 2020;383(2):120-128. doi:10.1056/NEJMoa2015432
- Bompard F, Monnier H, Saab I, et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J. Jul 2020;56(1)doi:10.1183/13993003.01365-2020
- Criel M, Falter M, Jaeken J, et al. Venous thromboembolism in SARS-CoV-2 patients: only a problem in ventilated ICU patients, or is there more to it? Eur Respir J. Jul 2020;56(1)doi:10.1183/13993003.01201-2020
- Poor HD, Ventetuolo CE, Tolbert T, et al. COVID-19 critical illness pathophysiology driven by diffuse pulmonary thrombi and pulmonary endothelial dysfunction responsive to thrombolysis. Clin Transl Med. Jun 2020;10(2):e44. doi:10.1002/ctm2.44
- Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 05 15 2020;201(10):1299-1300. doi:10.1164/rccm.202003-0817LE
- Guignabert C, Phan C, Seferian A, et al. Dasatinib induces lung vascular toxicity and predisposes to pulmonary hypertension. J Clin Invest. 09 01 2016;126(9):3207-18. doi:10.1172/JCI86249
- Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 05 02 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”