American Heart Association Early Career Guest Blog
Sherry-Ann Brown MD PhD FAHA, Krishna Doshi BS
We cannot ignore what a recent president of the World Medical Association describes as the “physician burnout pandemic”. We must find ways to transform our professional lives from a state of burnout to a state of wellness. A study from the American College of Cardiology reported that 27% of cardiologists experience burnout (compared to 43% from Medscape), while 49.5% reported being under stress with limited energy (1). In another study, approximately 15% of cardiologists reported experiencing depression, and among these 33% easily became exasperated by patients and 32% felt less engaged with patients (2). Similarly, burned-out physicians noted an effect on their professional activities with both patients and colleagues (1).
Neither subspecialty nor practice setting appears to have an impact on burnout (1). Contributors to burnout among cardiologists have been listed as excessive workloads, large bureaucratic loads, balancing work and life, and after work emergencies impacting lifestyle (1)(2). The constantly evolving technology was also identified as a culprit, with 57% of cardiologists reportedly accessing the electronic medical record at home (1)(4). I think we may all be guilty of some of this. Further, in the era of COVID-19, most of our professional and social interactions have been transferred to virtual interfaces. The absence of physical togetherness can take its toll on our emotional or mental wellness, coupled with decreased social support for many in the pandemic (5).
One cardiologist wrote in a survey that our profession is the ‘most unhappy’ specialty, but also the least likely to seek professional help. Thus, to cope many physicians turn to food, alcohol, drugs, or smoking (2). The struggle is real across our professions, and we must as a society pursue recommendations for burnout mitigation strategies (4). These initiatives must be conducted in shared responsibility for physician wellness (4). Resilience-based interventions should consider job design, leadership, and management training (4), and must be endorsed by the C-suite, with commitment to broad-sweeping implantation across the institution. Reduction in administrative tasks for physicians, increasing non-physician support staff, and emphasizing teamwork can make a world of difference, as can fostering self-awareness, life-work balance or more aptly integration, and regular check-ins for mental health (4).
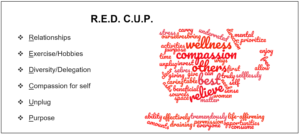
R.E.D. C.U.P.
To avoid or overcome being in a state of burnout, there are key components of the journey to wellness that should also be embraced.
Relationships
When we informally survey individuals in person or on social media, undoubtedly the number one catalyst for wellness is noted as relationships. Frequent personal interactions with others who know and understand us can help relieve some of the altruistic burdens we carry in our daily professional lives.
Exercise/Hobbies
Quite often exercise and hobbies are listed as mediators of wellness. Exercise can relieve stress and release endorphins that help improve mood. Hobbies can give an object of focus that takes our minds away from what troubles us, or perhaps what might otherwise consume or overwhelm us. Hobbies can also help us share our inner selves, interests, and creative skills with others.
Diversity/Delegate
Welcoming a diversity of perspectives and selectively delegating to individuals with the appropriate level of training and preparation can offload some of the pressure on our generally full plates. Surrounding yourselves with individuals who enjoy taking initiative and being resourceful can be mutually beneficial.
Compassion for self
Giving yourself permission to have compassion for yourself is tremendously underrated, especially by women. We are so used to caring for everyone else around us and sharing our compassion selflessly that we often forget to do so for ourselves. To bring our best selves to the table and to truly give our best to others, we need to first invest in our own selves in ways that matter most to each of us.
Unplug
The ability to intermittently unplug from sources of time-consuming or draining asks can free up incredible amounts of time and mental space that can be used on more enriching and life-affirming activities.
Purpose
A sense of purpose can give clear direction and allow us to prioritize opportunities more effectively.
Pursuing R.E.D. C.U.P. may help us collectively and collaboratively as we grow together on our journey from burnout to wellness.
References:
- Mehta LS, Lewis SJ, Duvernoy CS, Rzeszut AK, Walsh MN, Harrington RA, et al. Burnout and Career Satisfaction Among U.S. Cardiologists. J Am Coll Cardiol. 2019;73(25):3345-8.
- Nicholls M. Cardiologists and the Burnout scenario. Eur Heart J. 2019;40(1):5-6.
- Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320(11):1131-50.
- Panagioti M, Geraghty K, Johnson J. How to prevent burnout in cardiologists? A review of the current evidence, gaps, and future directions. Trends Cardiovasc Med. 2018;28(1):1-7.
- Graham MM, Higginson L, Brindley PG, Jetly R. Feel Better, Work Better: The COVID-19 Perspective. Can J Cardiol. 2020;36(6):789-91.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”