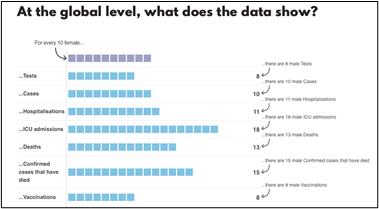
Fig1: Data source: The sex, Gender and Covid-19 Project. (https://globalhealth5050.org/the-sex-gender-and-covid-19-project/about-us/)
As we just passed our first anniversary of fighting COVID-19, we are in a better position than we used to be a year ago. Nationwide vaccine efforts encourage us to see the light at the end of the tunnel. However, the virus is still lurking around and always finds its way back in many unpredictable forms as it evolves rapidly. We need to stay vigilant and use what we learned from the previous years’ knowledge to guide us defend any future attacks. One pertinent piece of information we discovered is that COVID-19 attacks us unequally. People are over 65 years old and people with any underlying complications are more at risk. Another important discovery is that there is a sex difference in infection, severity, and death among women and men.
In most countries, the incidence of infection (percent of cases) is similar in both sexes. However, men consistently develop more serious symptoms and have more mortalities across age groups on a global level (Fig1). More specifically, men account for about 59% to 75% of total mortality1. It’s indisputable that sex is an important factor when it comes to understand and combat COVID-19. Here are a couple of candidate mechanisms potentially contributing to sex-biased COVID-19 mortality.
Hormones
Many sex differences in the manifestation of disease development have long been attributed to sex hormones, particularly in the realm of immune responses. Both innate and adaptive immune responses are affected by sex-dependent factors2. Males are more susceptible to infections caused by parasites, fungi, bacteria, and viruses, one of the possible determining factors is sex hormone3. More specifically, the immune-suppressive androgens reside in males and immune protective estrogens reside in females. Females might produce more antibodies and launch a stronger immune defense to infection because of estrogens, while males lack the advantage to react the same way. Female hormones, estrogens, can ameliorate the severity of influenza infections by suppressing pro-inflammatory responses in mice4. The anti-inflammatory activity of estrogen is potentially through the regulation of the SOCS3 and STAT3 signaling pathways, specifically to promote the progression of the anti-inflammatory process towards the IL-10-dependent pathway in macrophages5. Sex hormones can regulate the immune response via regulating circadian rhythm, microbial composition, and transcriptional regulation such as estrogen receptors (ERs) and peroxisome proliferator-activated receptors (PPARs)6.
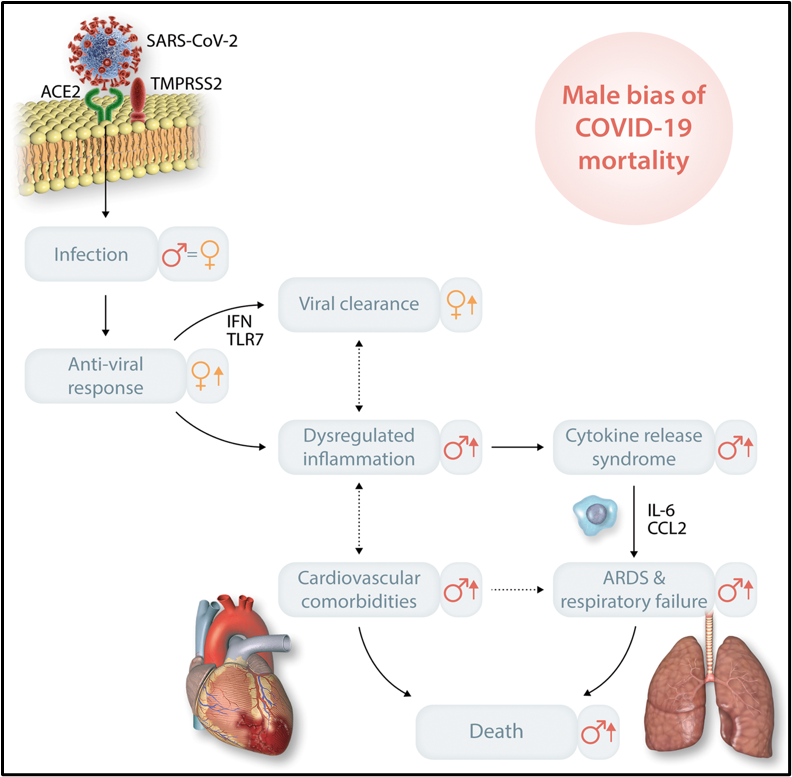
Fig2: Potential mechanisms of male bias of COVID-19 mortality7.
Sex chromosomes
One of the fundamental differences between men and women is the X and Y sex chromosomes. Females have two X chromosomes with a functional one and an inactive one to maintain the balance of chromosomal X gene dosage, while males only have one functional X chromosome and one Y chromosome to maintain the identity of sex-specific effects and testis development. This evolutional advantage in females provides a “back-up” plan in case of a “disease gene” on X chromosome inherited from either the maternal or paternal side. Some genes can escape from X chromosomal inactivation and consequently express higher levels. The gene encoding a receptor that is responsible for SAS-CoV-2 virus cellular entry is called ACE2. ACE2 locates at X chromosome and is potentially a target for ineffective chromosome inactivation, and which could cause a female-biased increased level of ACE2 expression7. A higher level of ACE2 in females promotes viral clearance. On the contrary, a lower level of ACE2 causes dysregulated inflammation, increased cardiovascular comorbidities, increased risk of respiratory failure in males7 (Fig2). Other inflammatory response-related genes on the X chromosome include pattern recognition receptors such as toll-like receptor 7 (TLR7), TLR8, interleukin-1 receptor-associated genes, and NFKB essential modulator genes8. Additionally, it has been shown that TLR3, TLR7, and TLR9 are female-biased while TLR2 and TLR4 are male-biased. These differences potentially reveal why males and females respond to infection differently7,8. The research on understanding sex dimorphisms in immunity is critical to help us fight COVID-19 more effectively.
In conclusion, strong evidence shows that COVID-19 affects men and women unequally. Aside from socio-economic, lifestyle and environmental differences, biology plays an important role in male-biased COVID-19 severity and mortality. To understand and combat infection more precisely, we need to consider sex as a biological variable and develop therapeutic strategies for men and women respectively.
References
- Griffith DM, Sharma G, Holliday CS, Enyia OK, Valliere M, Semlow AR, Stewart EC, Blumenthal RS. Men and COVID-19: A Biopsychosocial Approach to Understanding Sex Differences in Mortality and Recommendations for Practice and Policy Interventions. Preventing chronic disease. 2020;17:E63.
- Markle JG, Fish EN. SeXX matters in immunity. Trends in Immunology. 2014;35(3):97–104.
- Klein SL. The effects of hormones on sex differences in infection: from genes to behavior. Neuroscience & Biobehavioral Reviews. 2000;24(6):627–638.
- Robinson DP, Lorenzo ME, Jian W, Klein SL. Elevated 17β-Estradiol Protects Females from Influenza A Virus Pathogenesis by Suppressing Inflammatory Responses. PLOS Pathogens. 2011;7(7):e1002149.
- Villa A, Rizzi N, Vegeto E, Ciana P, Maggi A. Estrogen accelerates the resolution of inflammation in macrophagic cells. Scientific Reports. 2015;5(1):15224.
- Taneja V. Sex Hormones Determine Immune Response. Frontiers in immunology. 2018;9:1931.
- Bienvenu LA, Noonan J, Wang X, Peter K. Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovascular Research. 2020;116(14):2197–2206.
- Pradhan A, Olsson P-E. Sex differences in severity and mortality from COVID-19: are males more vulnerable? Biology of Sex Differences. 2020;11(1):53.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”