Amongst the uncertainty of the future and how this pandemic will end, there comes a huge responsibility on all healthcare workers to care for the sickest patients while staying safe, to lead their healthcare systems and to come together as one unit against this crisis. Seeing how this pandemic has affected our healthcare system, from the evolving utility of telehealth to canceling elective procedures in multiple specialties, I decided to share a few thoughts on COVID-19 and the cardiovascular manifestations associated with this infection and how COVID-19 has affected our approach to commonly performed procedures in the cardiac catheterization lab.
Cardiovascular manifestations of COVID-19
Although coronavirus predominantly affects the respiratory system, causing a variety of symptoms from flu-like symptoms to acute respiratory failure requiring intubation, it can affect other organs, and patients may present with non-respiratory complaints [1]. The cardiovascular manifestations of COVID-19 have a wide range of clinical presentations (Figure 1), from pericarditis, myocarditis, pericardial effusion, and decompensated heart failure to tamponade, cardiogenic shock and ST-elevation myocardial infarction (STEMI) [1-2]. In addition, right ventricular strain should raise suspicion for pulmonary embolism as these infected patients tend to be hyper-coagulable with a high incidence of venous thromboembolism for currently unclear reasons. It is important to recognize these cardiovascular manifestations of COVID-19, as it is thought that cardiovascular involvement is associated with a worse prognosis [1].
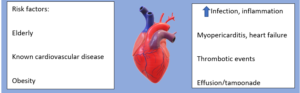
Figure 1: Potential risk factors and cardiovascular manifestations of COVID-19 patients.
Approach to Acute Coronary Syndrome (ACS) and Structural Procedures in the Cath Lab in COVID-19 Pandemic
Like any procedural field, interventional cardiology has been affected by this pandemic. All elective procedures are being postponed until the crisis settles down per recommendations from the Centers for Disease Control and Prevention (CDC), with emergent, urgent, time-sensitive procedures still being performed, in an attempt to preserve hospital beds and personal protective equipment (PPE) for COVID-19 patients [2]. This pandemic has led to several changes in the ACS approach across the world, with the main goal of reducing un-necessary exposure to health care workers and limiting the spread of this highly contagious disease [1,2].
To summarize, some of the key changes many hospitals have applied in their approach to some of the most commonly performed percutaneous cardiac procedures in COVID-19 patients:
- ACS patients
- Thrombolytics are considered standard therapy in many hospitals for many STEMI patients with symptoms <12 hours and no contraindications: signs of success are resolution of symptoms and/or >50% decrease in ST elevation. If thrombolytics fail, coronary angiogram and percutaneous coronary intervention (PCI) should be considered in an isolated cath lab (Figure 2) and the benefit versus the exposure risk should be carefully evaluated.
- For patients with low risk Non-ST elevation myocardial infarction (NSTEMI): medical therapy is reasonable. For those with high risk NSTEMI or failure of medical treatment, coronary angiogram and/or PCI should be performed. These coronary procedures are usually performed in isolated cath labs with only limited staff in the cath lab room, to avoid unnecessary exposure (Figure 2).
- Structural heart disease patients
- For patients who are unstable and have severe aortic stenosis (AS), balloon aortic valvuloplasty (BAV) should be performed emergently to stabilize the patient if this is thought to be the cause of the hemodynamic instability. For those who develop significant aortic regurgitation after BAV, transcatheter aortic valve replacement (TAVR) should be performed.
- Patients with severe symptomatic AS, TAVR is considered a time-sensitive procedure. The benefit of TAVR and risk of infection exposure should be discussed.It is important to note that this change in policy, in part, could explain the decrease in cath lab activation rates for STEMI during this pandemic [2]; as many STEMI patients are receiving thrombolytics. In addition to that, many patients are not seeking medical care, or if they do, they are presenting late, possibly due to fear from contracting the virus in the hospital, potentially leading to late STEMI complications [2]. Thus, it is important to counsel our patients in our virtual clinic visits that if significant symptoms develop, they should seek medical care.
Lastly, I want to thank all of my colleagues and healthcare workers across the nation and across the globe for risking their lives for patients and for their continued dedication. This is a critical time for everyone in the health care system. In light of this pandemic, I hope we continue to learn and share our experiences in this global crisis in order to improve our patient’s care, safety for our healthcare workers and the dynamics of our healthcare system.
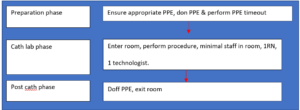
Figure 2: Simplified Set-up of an Isolated Cath Lab during the COVID-19 pandemic.
References
- Fried et al: The Variety of Cardiovascular Presentations of COVID-19. 2020 Apr 3. doi: 10.1161/CIRCULATIONAHA.120.047164. [Epub ahead of print] https://www.ncbi.nlm.nih.gov/pubmed/32243205
- Garcia et al: Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020 Apr 10. Epublished DOI:10.1016/j.jacc.2020.04.011 http://www.onlinejacc.org/content/early/2020/04/07/j.jacc.2020.04.011
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”