As a 3rd year medical student in the coronary care unit (CCU), I helped care for a patient whose story I will never forget. She had developed advanced heart failure due to peripartum cardiomyopathy in her 20s giving birth to her only child and required a heart transplant. She did well for a number of years, but I met her in her 30s when she was admitted post-MI in cardiogenic shock. Her coronary atherosclerosis was due to severe coronary allograft vasculopathy (CAV), an aggressive form of CAD transplant patients may develop. She got a LAD stent and was supported with a balloon pump but was tenuous at best. Some days after her PCI, in a moment seared into my memory, she let out an ear-piercing yell and suddenly arrested and died, her daughter at the bedside. I’ll always remember the pain on her child’s face when she passed, and I will always have a sincere appreciation for the misery CAV can cause. This blog is meant to provide some historical context to heart transplantation and the issue of CAV, as well as to discuss ways we can prevent it.
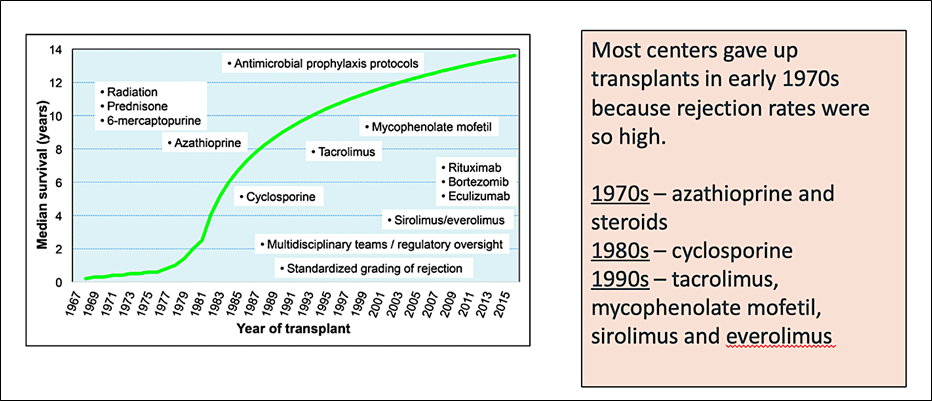
Since the first heart transplant in Cape Town, South Africa, there have been tremendous advances in cardiac transplantation with median survival now around 12 years. It didn’t always appear that this would be the case, with mortality so high in the early days that many felt heart transplant wasn’t worth it. The advent of calcineurin inhibitors with cyclosporine in the 1980s and tacrolimus in the 1990s were key (Figure 1). Steady improvements in infection prophylaxis, screening for and treating rejection, and surgical technique and expertise further helped the cause.
But as we addressed one set of problems, we found another. CAV is an aggressive form of coronary artery disease (CAD) present in 30% of heart transplant recipients at 5 years and 50% at 10 years. Those with it have worse survival. It shares some risk factors with classic CAD but has several of its own, and there are key pathophysiologic differences (Figures 2 and 3). Our patient was unique in that she had a true plaque rupture MI, typically occurring less often with CAV relative to classic CAD, but this may have been related to a donor transmitted lesion acting more as typical CAD would.
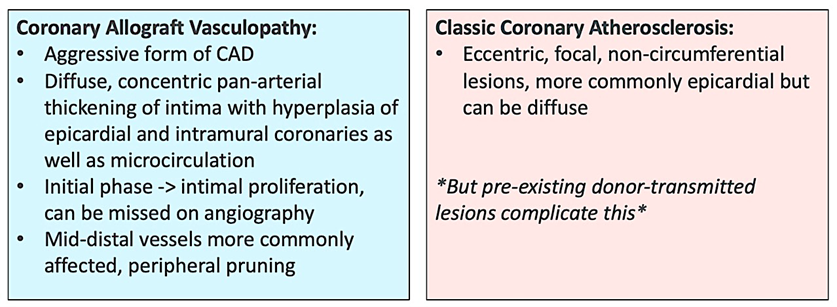
Figure 2. Pathophysiologic Differences
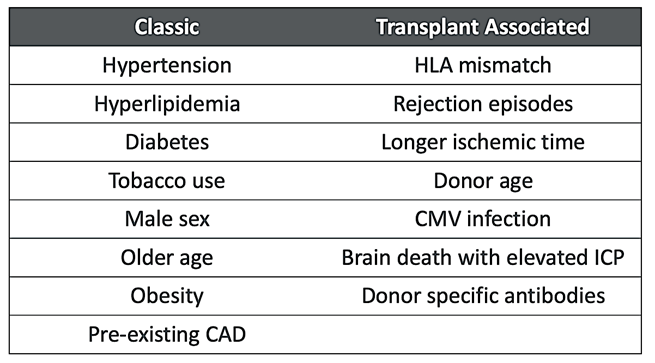
Figure 3. Risk Factors
So how do we prevent CAV? Our best data comes from statin trials in the 1990s-2000s (pravastatin, simvastatin, and atorvastatin studied), showing lower rates of rejection and CAV with improved survival in transplant patients treated with statins. This makes intuitive sense, as dyslipidemia is a rock-solid risk factor for classic CAD and nearly universally seen post solid organ transplantation due to the metabolic consequences of common immunosuppressives. These immunosuppressives, while life-saving in their own right, also lead to worsening glucose control, hypertension, obesity, and kidney disease. Addressing each of these while encouraging a heart-healthy diet and routine exercise is of paramount importance in keeping our transplant patients healthy. Finally, a reminder that there are many drug-drug interactions with transplant medications. Figure 4 is adapted from Warden et al and shows the relative degree of interactions between immunosuppressives and common lipid-lowering drugs.
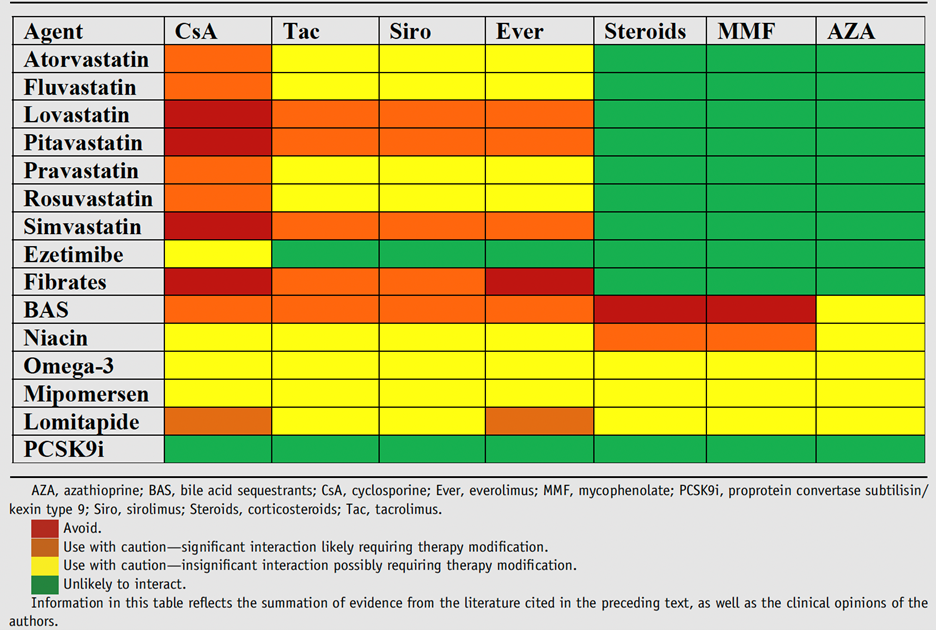
Figure 4. Drug-Drug Interactions
While this story was tragic for the patient and her family, it’s given me a profound respect for CAV that I will carry forward when I eventually care for heart transplant patients in my career. Below are the references for this article from which parts of the figures were taken. Each of these is a fantastic resource for further learning.
References:
- Stehlik, J., et al. (2018). “Honoring 50 Years of Clinical Heart Transplantation in Circulation: In-Depth State-of-the-Art Review.” Circulation 137(1): 71-87.
- Warden, B. A. and P. B. Duell (2019). “Management of dyslipidemia in adult solid organ transplant recipients.” J Clin Lipidol 13(2): 231-245.
- Costanzo, M. R., et al. (2010). “The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients.” J Heart Lung Transplant 29(8): 914-956.