For the heart’s health condition, everything is interconnected. Other parts of the body might be reflective or instigators of a failing heart. Among all of the important issues related to cardiovascular disease, skeletal muscle is on top of that list. Conventionally, the main function of skeletal muscle is tightly related to physical capabilities. It’s only the partial facts. Skeletal muscle plays a pivotal role in supporting our physical well-being in many ways that are more than organizational. The relationship between skeletal muscle mass and cardiometabolic health starts to attract the researcher’s attention.
 As we know, skeletal muscle mass decreases during the aging process, while cardiometabolic health often declines. A recently published epidemiology study investigated the relationship between skeletal muscle mass and cardiovascular disease in a group of adults (3042 people) without pre-existing cardiovascular risk in a 10-year follow-up study, ATTICA1. After adjusting for various confounders, this study showed a significant inverse association between skeletal muscle mass and cardiovascular incidence (HR 0.06, 95% CI 0.005 to 0.78). Moreover, it showed that people in the highest skeletal muscle mass group had 81% lower risk for a cardiovascular event. The results are quite intriguing. Does decreased skeletal muscle mass contribute to poor heart health or does a failing heart cause muscle mass decrease? It’s hard to figure out the cause and effect without understanding the relationship between skeletal muscle and the heart.
As we know, skeletal muscle mass decreases during the aging process, while cardiometabolic health often declines. A recently published epidemiology study investigated the relationship between skeletal muscle mass and cardiovascular disease in a group of adults (3042 people) without pre-existing cardiovascular risk in a 10-year follow-up study, ATTICA1. After adjusting for various confounders, this study showed a significant inverse association between skeletal muscle mass and cardiovascular incidence (HR 0.06, 95% CI 0.005 to 0.78). Moreover, it showed that people in the highest skeletal muscle mass group had 81% lower risk for a cardiovascular event. The results are quite intriguing. Does decreased skeletal muscle mass contribute to poor heart health or does a failing heart cause muscle mass decrease? It’s hard to figure out the cause and effect without understanding the relationship between skeletal muscle and the heart.
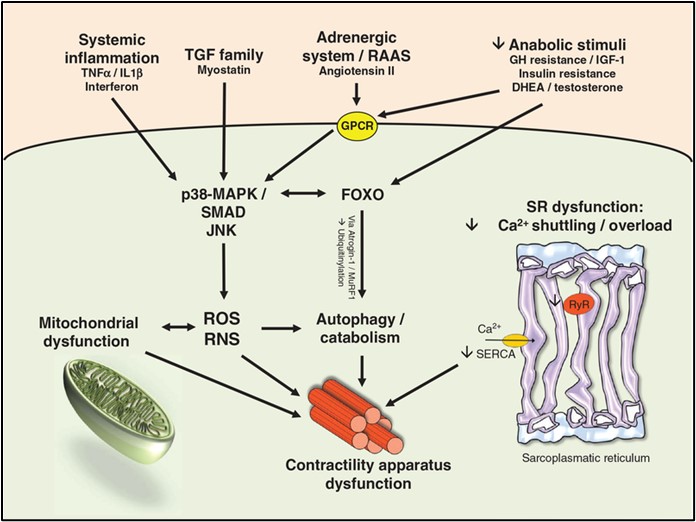
Chronic heart diseases and heart failure impair muscle function2. In particular, many heart diseases affect exercise performance. For certain cardiac conditions such as atherosclerotic heart disease, exercise stress test is widely used to measure heart functional capacity, and also used as a diagnostic tool to evaluate the efficacy of treatment and predict prognosis. Cardiac function affects exercise performance in many ways and reduced cardiac output response to exercise leading to skeletal muscle hypoperfusion and lactic acidosis3. The pathophysiological mechanisms impairing skeletal muscle function in heart failure are discussed in a review, shown in Fig12. In heart failure, many stimuli contribute to skeletal muscle contractility apparatus dysfunction such as systemic inflammation, TGF family members, adrenergic signaling, decreased anabolic stimuli and increased calcium shuttling/overload (Fig. 1). Skeletal muscle atrophy can be caused by biological processes such as protein degradation, impaired growth factor signaling and skeletal muscle inflammation.
Heart failure with increased systemic inflammation can trigger skeletal muscle inflammation. it’s also true the other way around: skeletal muscle injury can cause local activation of innate immune system4. Danger-associated molecular patterns (DAMPs) can be released from dying myocytes. DAMPs encompass diverse mediators including alarmins (HMGB1, S100A8/9/12, S100B, IL1a, HSPs), bioactive lipids, extracellular matrix fragments and nucleotides (ATP, CpG, dsRNA)5. The impact of local skeletal muscle immune responses has been proved both harmful and beneficial. Traditionally, a stimulated immune response (M1-like macrophages) is a sign of disease. However, distinct macrophage subsets (M2-like macrophages) help tissue regeneration in chronic skeletal muscle pathologies6. The relationship between skeletal muscle damage and inflammation is complicated. And how they play a role in heart diseases require more research in the future.
To go back to the original question in this blog, the answer is a yes. Yes, skeletal muscle (leg and arm muscle) can tell the basic condition of the heart. And is it good for your heart if there is more muscle mass? Maybe. The absolute muscle mass does not tell us the function of the muscle, other aspects of muscle, for example, different types of fiber may hold the key.
References
- Tyrovolas S, Panagiotakos D, Georgousopoulou E, Chrysohoou C, Tousoulis D, Haro JM, Pitsavos C. Skeletal muscle mass in relation to 10 year cardiovascular disease incidence among middle aged and older adults: the ATTICA study. Journal of Epidemiology and Community Health. 2020;74(1):26 LP – 31.
- Kennel PJ, Mancini DM, Schulze PC. Skeletal Muscle Changes in Chronic Cardiac Disease and Failure. Comprehensive Physiology. 2015;5(4):1947–1969.
- Lunde PK, Sjaastad I, Schiøtz Thorud H-M, Sejersted OM. Skeletal muscle disorders in heart failure. Acta Physiologica Scandinavica. 2001;171(3):277–294.
- Lavine KJ, Sierra OL. Skeletal muscle inflammation and atrophy in heart failure. Heart failure reviews. 2017;22(2):179–189.
- Chan JK, Roth J, Oppenheim JJ, Tracey KJ, Vogl T, Feldmann M, Horwood N, Nanchahal J. Alarmins: awaiting a clinical response. The Journal of Clinical Investigation. 2012;122(8):2711–2719.
- Villalta SA, Deng B, Rinaldi C, Wehling-Henricks M, Tidball JG. IFN-γ Promotes Muscle Damage in the <em>mdx</em> Mouse Model of Duchenne Muscular Dystrophy by Suppressing M2 Macrophage Activation and Inhibiting Muscle Cell Proliferation. The Journal of Immunology. 2011;187(10):5419 LP – 5428.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”