As part of its mission to be a relentless force for a world of longer, healthier lives, the American Heart Association (AHA) has been working diligently to eliminate barriers to health equity in the U.S. diverse population through education and research, raising awareness through their many programs and initiatives. In the stroke arena, we continue to face significant inequities related to stroke incidence, prevalence, care, and outcomes in ethnic minorities.1 Consequently, there has been a number of initiatives launched to address these disparities. The Health Equity and Actionable Disparities in Stroke Symposium, a collaborative initiative of the American Heart Association and National Institute of Neurological Disorders and Stroke, took place in 2020 with the goals of reducing inequities in stroke care and research. It also aimed to accelerate the translation of research findings to improve outcomes for racial and ethnic minorities.1
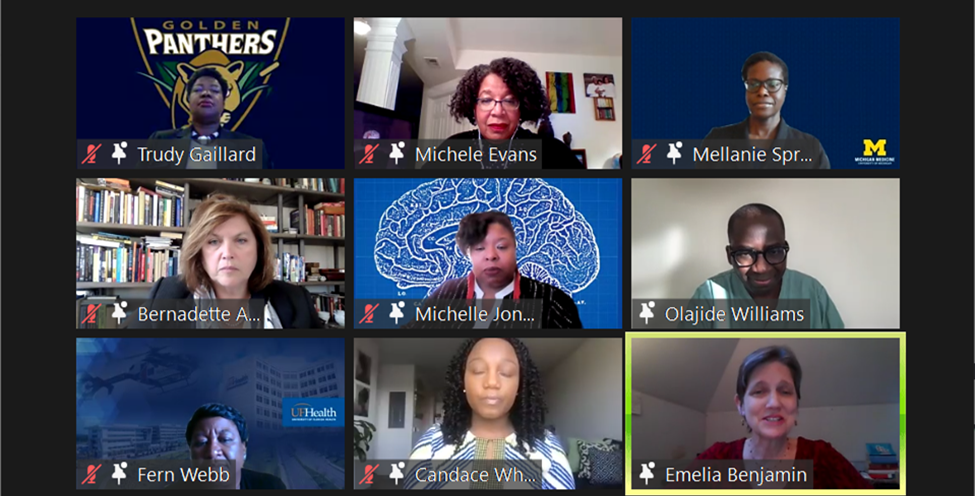
This year the American Heart Association continues the efforts to promote awareness of the importance of diversity and inclusion in stroke science. A roundtable session took place on Friday, March 17, during the last day of the prestigious 2021 International Stroke Conference. A panel of experts shared their views and presented alternatives to improve diversity and Inclusion in the healthcare workforce, clinical trial enrollment, and community engagement. The expert roundtable included experts in the field such as Dr. Emelia Benjamin, MD ScM FAHA, Michele Evans, MD, Michelle Jones-London, Ph.D., Bernadette Boden-Albala, MD MPH, Fern Webb, Ph.D., Candace Whitfield, BS, Trudy Gaillard, RN Ph.D., Mellanie Springer, MD MSc. Mr. Olajide Williams, MS served as the moderator of the roundtable. The panelists presented a fresh and clear view of the diversity and inclusion barriers encountered in the research arena. They also offered alternatives to support inclusion and diversity in the development of research protocols, proposal procedures through institutional review boards, and through community engagement, with the use of community-based participatory research.
The experts highlighted the issue of representativeness in the conduct of research and presented diversity as a solution. Diversity in research means that people of different ages, different racial and ethnic groups and both men and women participate in research studies. The lack of diversity in participants of research impedes the ability to generalize study results and make medical advancements of effective therapies. It may further prevent some populations from experiencing the benefits of research innovations and receipt of high-quality care.2
In the context of clinical trial enrollment, the speakers emphasized the importance of having a diverse sample. They also discussed the need for inclusivity of minority groups during the enrollment period. They also highlighted the importance of informed consent forms available in other languages to facilitate the diversity of the sample during enrollment. They also suggested the approval of translated informed consent forms in an expedited fashion to avoid delays in the consenting process for ethnic minority groups. Another very important factor was the importance of having the infrastructure to support diversity and inclusion in the stroke science workforce. Factors such as the hiring of clinicians and research personnel that may resemble the target population of interest are vital to facilitate the recruitment of ethnic minority groups much needed in these studies.3
As academicians and researchers, we should advocate for diversity as it drives excellence and enhances innovation in the biomedical sciences, leading to novel findings and treatment of diverse populations.3 Diverse and inclusive scientific teams can generate new research questions, develop methodical and analytical approaches to better understand study populations, and offer approaches to problem-solving from multiple and different perspectives. Moreover, the promotion of diverse groups presents opportunities for the inclusion of individuals with different perspectives who can complement each other and inform of new approaches.3 This may further strengthen the approach of the research team through the various phases of the research process, especially when their diversity and inclusion match the racial and ethnic minority group under study.
One of the experts, Dr. Michelle Evans highlighted the importance of community-based participatory engagement in research, especially in ethnic minorities. Another speaker, Dr. Trudy Gaillard discussed the opportunity to engage members in the community, stakeholders, and utilize this as a venue to engage study participants through community-based participatory research (CBPR). Engaging in active reflection and adopting promising partnering practices are important for CBPR partnerships working to improve health equity.4
The roundtable presentation aligns with current National Institutes of Health (NIH) strategies to support diversity and inclusion in the science community. A program called UNITE was launched in 2020 to tackle the problem of racism and discrimination in science while developing methods to promote diversity and inclusion across the biomedical enterprise. Some of its functions include understanding stakeholder experiences through listening and learning, pursuing research on health disparities, minority health, and health equity, improving the NIH culture and structure for equity, inclusion and excellence, transparency, communication, and accountability with internal and external stakeholders, changing policy, culture, and structure to promote workforce diversity (NIH, 2021).5
In addition to NIH, the National Institute of Neurological Disorders and Stroke (NINDS) (2021) is committing to diversity, equity, and inclusion in the neuroscience community as both an employer and funding agency, addressing the stark differences in neurological health outcomes related to where one lives, has access to care, their race/ethnicity, and socioeconomic status.6 In the process of implementation of these initiatives, it will be important to note that implementation science can exacerbate health disparities if its use is biased toward entities that already have the highest capacities for delivering evidence-based interventions.
There is a call for making efficient use of existing data by applying epidemiologic and simulation modeling to understand what drives disparities and how these can be overcome. There is also a need for designing new research studies that include populations experiencing disparities in cardiovascular disease, neurological disease, and stroke.7 It will be interesting to observe in the next coming months, the implementation of some of these strategies to promote diversity and inclusion in stroke science. Much remains to be done to bridge the gap and reduce healthcare-related disparities in racial-ethnic minority groups, especially in the context of stroke science. In the meantime, it is up to us to continue the work of raising awareness, promoting diversity and inclusion in our academic circles, in the science field, and in our communities.
For additional information on the efforts American Heart Association to support diversity and inclusion in heart science, please be sure to check out https://www.heart.org/en/about-us/diversity-inclusion.
References:
- Towfighi A, Benson RT, Tagge R, Moy CS, Wright CB, Ovbiagele B. Inaugural Health Equity and Actionable Disparities in Stroke: Understanding and Problem-Solving Symposium. Stroke. 2020;51(11):3382-3391. doi:10.1161/STROKEAHA.120.030423
- University of Maryland. Health Equity Project. (2021). Top five reasons why diversity is important in research. Retrieved from https://buildingtrustumd.org/unit/importance-of-research/importance-of-diversity#:~:text=Diversity%20in%20research%20means%20that%20people%20of%20different,specific%20reasons%20why%20diversity%20in%20research%20is%20important.
- Swartz TH, Palermo AS, Masur SK, Aberg JA. The Science and Value of Diversity: Closing the Gaps in Our Understanding of Inclusion and Diversity. J Infect Dis. 2019;220(220 Suppl 2):S33-S41. doi:10.1093/infdis/jiz174
- Dickson E, Magarati M, Boursaw B, et al. Characteristics and Practices Within Research Partnerships for Health and Social Equity. Nurs Res. 2020;69(1):51-61. doi:10.1097/NNR.0000000000000399
- National Institutes of Health. (NIH). (2021). Ending Structural Racism. Retrieved from https://www.nih.gov/ending-structural-racism/unite on 4/2/21.
- National NINDS (2021). NINDS is committed to ending structural racism. Retrieved from https://www.ninds.nih.gov/News-Events/Directors-Messages/All-Directors-Messages/NINDS-committed-ending-structural-racism
- McNulty M, Smith JD, Villamar J, et al. Implementation Research Methodologies for Achieving Scientific Equity and Health Equity. Ethn Dis. 2019;29(Suppl 1):83-92. Published 2019 Feb 21. doi:10.18865/ed.29.S1.83
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”